Foire Aux Questions
À propos de la psychologie
L’Ordre des psychologues de l’Ontario (l’Ordre) réglemente la profession de psychologue dans la province. Les membres de l’Ordre sont des professionnels réglementés et sont les seules personnes autorisées à exercer la psychologie en Ontario. Les psychologues et les associés en psychologie sont membres de l’Ordre.
L’Ordre n’est pas une université, ni un collège communautaire, ni une école. Il a pour mandat de protéger l’intérêt du public en voyant à ce que les consommateurs reçoivent des services psychologiques professionnels et éthiques donnés par des fournisseurs compétents et qualifiés.
Les professionnels réglementés sont tenus par la loi de fournir des services d’une manière compétente et éthique. Parce que leur profession est régie par un organisme de réglementation, ils sont responsables envers le public de leurs activités et de leurs comportements professionnels. Étant membres de l’Ordre des psychologues de l’Ontario, les psychologues et les associés en psychologie doivent se conformer à des exigences rigoureuses d’entrée dans la profession, respecter les normes, lignes directrices et principes éthiques prescrits, et participer à des activités d’assurance de la qualité pour continuellement se tenir à jour et améliorer leurs connaissances et leurs compétences.
Par ailleurs, l’Ordre n’a aucun pouvoir sur les fournisseurs de services non réglementés. Il n’existe aucun organisme de réglementation doté du pouvoir d’établir les exigences minimales d’éducation, de formation et de compétence ou d’établir et de surveiller les normes de conduite professionnelle et éthique des fournisseurs non réglementés. Il n’existe aucun organisme de réglementation chargé de protéger vos intérêts et de rendre les fournisseurs non réglementés responsables des services que vous recevez.
Seuls les membres de l’Ordre sont autorisés à employer le titre de « psychologue » ; ou d’« associé en psychologie » ; d’employer les termes « psychologie » ou ; « psychologique » dans la description des services qu’ils offrent ou fournissent; ou de se présenter comme des psychologues ou des associés en psychologie. Les psychologues et les associés en psychologie s’identifient également en ajoutant la désignation C. Psych. ou C. Psycho. Assoc. à la suite de leur nom.
Pour avoir le droit d’exercer la psychologie en qualité de professionnel inscrit, il faut avoir terminé avec succès des études universitaires de deuxième ou de troisième cycle en psychologie, avoir travaillé sous supervision professionnelle et avoir réussi aux examens. Les membres de l’Ordre doivent exercer la profession conformément aux lois, aux règlements, aux normes de conduite, aux lignes directrices professionnelles et aux codes de déontologie applicables.
Les psychologues et les associés en psychologie ont reçu une formation pour évaluer, traiter et prévenir les troubles comportementaux et mentaux. Ils diagnostiquent les troubles et les désordres neuropsychiques, psychotiques, névrotiques et de la personnalité. Ils utilisent toute une variété de méthodes pour maintenir et améliorer le fonctionnement physique, intellectuel, affectif, social et interpersonnel de leurs clients.
Les psychologues et les associés en psychologie choisissent habituellement de travailler dans un domaine particulier comme la psychologie clinique, la psychologie de counseling, la neuropsychologie clinique, la psychologie scolaire, la psychologie correctionnelle ou judiciaire, la psychologie de la santé, la psychologie en réadaptation ou la psychologie industrielle/organisationnelle. Les psychologues et les associés en psychologie qui travaillent dans ces domaines traitent toute une variété de populations clientes telles que les enfants, les adolescents, les adultes, les familles, les couples ou les organismes. Ils travaillent dans une variété de milieux, entre autres des écoles, des hôpitaux, des industries, des organismes de services sociaux, des établissements de réadaptation et des établissements correctionnels. Un grand nombre d’entre eux exercent également dans leur propre cabinet.
Les psychologues et les associés en psychologie qui sont titulaires d’un certificat d’inscription les autorisant à exercer de manière autonome peuvent fournir des services sans supervision dans leur domaine de compétence, et peuvent demander des honoraires pour ces services. Dans la plupart des cas, le certificat d’inscription des membres de l’Ordre n’est pas assorti de conditions ou de restrictions, mais ce n’est pas toujours le cas : les membres dont le certificat est assorti de conditions ou de restrictions doivent exercer conformément à ces conditions et restrictions.
L’Ordre tient un registre de tous ses membres actuels. Pour obtenir des renseignements sur un membre de l’Ordre, vous pouvez consulter le registre public en ligne ou en faire la demande auprès de l’Ordre par téléphone au 416-961-8817 ou par courriel à cpo@cpo.on.ca.
Les clients ont parfois besoin de faire signer des formulaires par leur psychologue ou leur associé en psychologie traitant pour que leur compagnie d’assurance leur rembourse le coût des services psychologiques ou pour avoir droit à certains avantages ou services offerts par un assureur ou un organisme gouvernemental. Normalement, les psychologues et les associés en psychologie sont autorisés à remplir et à signer ces formulaires. Si vous avez des questions à ce sujet, ou si vous avez de la difficulté à faire accepter ces formulaires, demandez conseil à l’Ordre.
La différence entre les psychologues et les associés en psychologie réside dans leur formation. Ils ont tous fait un baccalauréat, et ont tous fait des études de deuxième ou de troisième cycle en psychologie.
Les associés en psychologie ont obtenu une maîtrise en psychologie (p. ex. MA., MSc., MPs, MEd), puis ont travaillé pendant quatre ans dans le champ d’exercice de la psychologie. Les psychologues ont obtenu un doctorat en psychologie (PhD, PsyD, EdD, DPsy) et ont normalement fait un internat d’un an dans le cadre de leurs études.
Les psychologues et les associés en psychologie ont ensuite acquis au moins une année d’expérience de travail sous supervision approuvée par l’Ordre et ont réussi aux trois examens exigés par l’Ordre.
l'analyse comportementale appliquée (ACP)
Yes, the Peer Assessment may be conducted in-person or virtually. Any confidential documentation must be shared via a secure platform, and either anonymized or with the consent of the client.
Behaviour Analyst Transitional Route 2 applicants can download the Attestation A/B, Attestation C, and Peer Assessment Forms from the « Download Documents » section in the application portal or from the « Become a Member » section of the Reference Library.
Behaviour Analyst applicants must have the relevant organization submit the following supporting documents directly to the College: transcript(s), BACB® verification letter, and letters of good standing from other regulatory Colleges/Boards (if applicable).
E-mail is preferred: cpo@cpo.on.ca. If e-mail is not possible, please have the organization mail the document to:
The College of Psychologists of Ontario
110 Eglinton Ave West, Suite 500
Toronto, ON
M4R 1A3
Regarding the Vulnerable Sector Check, applicants may e-mail or upload it to their application form. Please contact the College if your region does not issue Vulnerable Sector Checks for registration purposes.
Yes, the incoming Psychology and Applied Behaviour Analysis Act (2021) requires Transitional Route 1 applicants to hold active BCBA® or BCBA-D® certification at the time that their certificate of registration authorizing autonomous practice as a Behaviour Analyst is issued by the College (i.e. from July 1, 2024 onwards). After an applicant receives their certificate from the College, they may decide to maintain their BCBA® or BCBA-D® certification or not. Registration will be the minimum requirement for practicing as a Behaviour Analyst, BACB® certification will be above and beyond registration.
Supervision is defined as:
…an ongoing educational, evaluative and hierarchical relationship, where the supervisee is required to comply with the direction of the supervisor, and the supervisor is responsible for the actions of the supervisee.
Supervision in ABA is a regulated professional service. The ABA supervisor is in a hierarchical relationship with their supervisees, whereby the supervisees must comply with the supervisor’s direction.
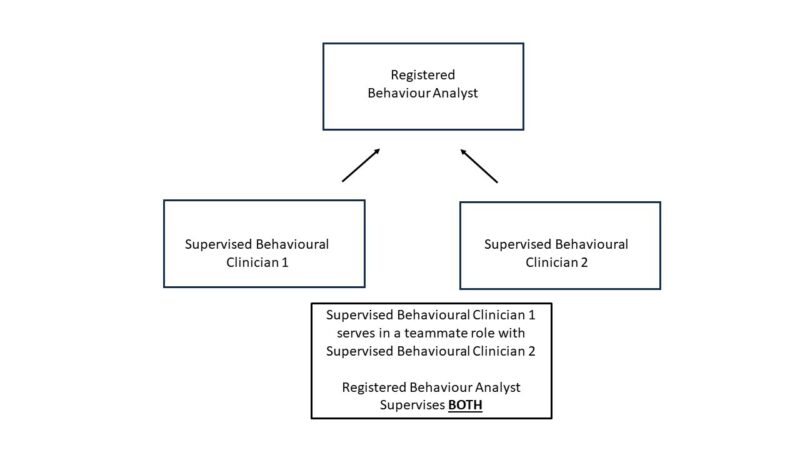
Models of care in ABA can sometimes include multiple teammates working together to serve a client’s needs.
The College does not permit “second-order” supervision. This means that, while a Behaviour Analyst’s supervisees may have varying roles and responsibilities as among themselves, including some oversight or supervisory roles, the Behaviour Analyst is directly responsible for all supervisees.
It may be helpful to think of the Behaviour Analyst as the one responsible for all services provided to the client. There may be multiple individuals involved in providing those services, who may have varying roles and responsibilities. The Behaviour Analyst is responsible for all the individuals involved in the provision of services to clients. The illustration above is meant to assist in emphasizing the Behaviour Analyst’s supervisory responsibilities across different models of care.
L’analyse comportementale appliquée (ACA) est l’application de la science de l’apprentissage pour comprendre et améliorer un comportement qui est significatif pour la personne et son entourage. L’ACA porte sur les effets que l’environnement peut avoir sur l’apprentissage. Le terme « comportement » désigne tout ce qu’une personne dit ou fait, y compris les aptitudes qu’il faut avoir et les actions qu’il faut faire pour parler, jouer et vivre. Le comportement peut aussi être privé (p. ex., les pensées et le ressenti).
L’ACA peut aider à augmenter des aptitudes utiles ou fonctionnelles (p. ex., la communication) ou à réduire des comportements nuisibles ou qui empêchent l’apprentissage (p. ex., l’automutilation).
L’intervention à l’aide de l’ACA utilise des procédés fondés sur des données probantes, tels que le renforcement positif, pour répondre aux inquiétudes et aux besoins d’un client, réduire les comportements nuisibles et augmenter les comportements désirables. Les analystes du comportement exercent dans toute une variété de milieux et auprès d’un grand nombre de populations clientes différentes.
Ressources :
- L’Ontario Association for Behaviour Analysis (ONTABA) a créé un graphique (en anglais) pour décrire ce qu’est l’ACA et ce qu’elle n’est pas. Le site Web de l’ONTABA renferme ce graphique et plus d’informations.
- Le site Web du Behavior Analysis Certification Board (BACB) présente d’autres informations au sujet de la profession d’analyste du comportement et des populations clientes qu’elle sert.
En 2017, le ministre de la Santé et des Soins de longue durée a demandé au Conseil consultatif de réglementation des professions de la santé de lui faire des recommandations sur les points suivants :
- Les activités ou les aspects associés à la thérapie par l’ACA qui posent un risque de préjudice important ou inhérent (le cas échéant), et si le risque de préjudice de cette thérapie varie selon la population cliente (p. ex., les enfants et les adultes); et
- Si l’ACA pose un risque, quelle série d’options peut-on considérer pour surveiller cette thérapie?
Dans son rapport intitulé Analyse appliquée du comportement : Risque de préjudice et supervision, présenté au ministre de la Santé et des Soins de longue durée en janvier 2018, le CCRPS tire la conclusion suivante :
« En se fondant les données probantes examinées, le CCRPS constate qu’il existe un risque de préjudice pour les clients associé à la plupart des interventions en ACA, et par conséquent, un travail de surveillance est recommandé. Plusieurs solutions de surveillance en matière de réglementation des fournisseurs ont été examinées, l’accent étant surtout mis sur les superviseurs cliniques. »
Pour ce qui est de la surveillance, voici ce que recommande le CCRPS :
« Dans sa recommandation, le CCRPS indique que le traitement par ACA pose de façon inhérente un risque de préjudice important auprès de nombreux groupes de clients. Par conséquent, le CCRPS recommande que les fournisseurs d’ACA qui exercent un rôle de supervision clinique (désignés tout au long de ce rapport comme les « superviseurs cliniques ») soient réglementés dans le cadre d’un ordre de réglementation des professionnels de la santé déjà établi, régi par la Loi de 1991 sur les professions de la santé réglementées (LPSR). D’autres fournisseurs d’ACA relèveraient de superviseurs cliniques réglementés. »
Pour protéger le public contre le risque de préjudice, les analystes du comportement qui supervisent ou fournissent des interventions en ACA devront respecter des normes clairement définies. Ces normes comprendront l’obligation d’avoir les connaissances, les compétences et le jugement nécessaires pour satisfaire aux exigences de la pratique et être autorisé à employer le titre réservé d’« analyste du comportement ».
Toute personne qui exerce une profession de la santé réglementée, qu’elle appartienne à la profession de psychologue, d’associé en psychologie, de médecin, d’infirmière, de dentiste, d’ergothérapeute ou à une autre profession de la santé réglementée, et maintenant à la profession d’analyste du comportement, doit être inscrite à un ordre de réglementation et être responsable devant cet ordre. Un ordre de réglementation n’est ni une université, ni un collège communautaire, ni une école. Il a plutôt pour mandat de protéger l’intérêt du public en veillant à ce que les clients reçoivent des services éthiques et professionnels donnés par des fournisseurs qualifiés et compétents.
L’Ontario compte 26 ordres de réglementation des professions de la santé, y compris l’Ordre des psychologues de l’Ontario. Pour obtenir plus d’informations et savoir comment et pourquoi les professions de la santé sont réglementées dans notre province, visitez le site Web de l’organisme Ontario Health Regulators.
La Loi stipule que les professionnels réglementés sont tenus de fournir des services professionnels, compétents et éthiques. Ils sont responsables devant le public de leur comportement et de leurs activités professionnels par le biais de l’organisme de réglementation auquel ils appartiennent. Lorsque les analystes du comportement seront réglementés, ils devront satisfaire à des normes rigoureuses d’entrée dans la profession, se conformer à des normes, des lignes directrices et des principes éthiques prescrits, et participer à des activités d’assurance de la qualité afin de continuellement mettre à jour et améliorer leurs connaissances et leurs compétences. Les processus de plainte et de discipline tiennent les professionnels responsables quand un client ou un autre membre du public allègue que les normes ont été enfreintes.
Par contre, l’Ordre n’a aucun pouvoir sur les fournisseurs de services non réglementés. Il n’existe aucun organisme de réglementation doté du pouvoir d’établir les normes minimales d’éducation, de formation et de compétence ou de surveiller les normes de conduite professionnelle et éthique des fournisseurs non réglementés. Aucun organisme de réglementation n’existe pour protéger votre intérêt et tenir les fournisseurs non réglementés responsables des services que vous recevez.
Le 3 juin 2021, la loi habilitante autorisant l’Ordre des psychologues de l’Ontario à réglementer la profession d’analyse comportementale appliquée (ACA), le projet de loi 283, Loi de 2021 visant à faire progresser la surveillance et la planification dans le cadre du système de santé de l’Ontario, a reçu la sanction royale. L’annexe 4 de ce projet de loi confère à l’Ordre le pouvoir de réglementer la profession d’analyste du comportement. La Loi sera proclamée par le gouvernement à un jour non encore fixé, révoquera la Loi de 1991 sur la psychologie et la remplacera par la Loi de 2021 sur la psychologie et l’analyse comportementale appliquée.
La nouvelle Loi prévoit que la réglementation de deux professions séparées et distinctes, celle de psychologie et celle d’analyse comportementale appliquée, sera régie par un seul ordre de réglementation. L’Ordre des psychologues de l’Ontario actuel réglementera les deux professions et son nom sera remplacé par celui d’Ordre des psychologues et des analystes du comportement de l’Ontario pour refléter son rôle élargi. La Loi maintient le cadre de réglementation des membres actuels de l’Ordre, c’est-à-dire les psychologues et les associés en psychologie, mais ajoute ce qui suit :
- Elle définit le champ d’exercice de l’ACA en ces termes : « L’exercice de l’analyse comportementale appliquée consiste, d’une part, dans l’évaluation du comportement caché et manifeste et de ses fonctions au moyen d’observations directes et de mesures et, d’autre part, dans la conception, la mise en œuvre, la prestation et l’évaluation d’interventions dérivées des principes du comportement afin de produire des améliorations significatives »;
- Élargit la restriction concernant la « déclaration de compétence » pour y inclure que nulle autre personne qu’un membre de l’Ordre ne doit se présenter comme une personne ayant qualité pour exercer en Ontario la profession d’analyste du comportement ou une spécialité de l’analyse comportementale appliquée;
- Restreint l’emploi du titre d’analyste du comportement aux membres inscrits au nouvel Ordre à titre d’analystes du comportement;
- Met à jour la grandeur et la composition du conseil de l’Ordre actuel afin que les deux professions puissent être représentées équitablement.
En 2017, à la demande du ministère de la Santé et des Soins de longue durée d’alors, le Conseil consultatif de réglementation des professions de la santé (CCRPS) a effectué une étude sur l’ACA, le risque de préjudice qu’elle pose et la nécessité de la réglementer. En réponse à une demande d’information, l’Ordre a envoyé une lettre énonçant, en partie, que si la décision est prise de réglementer l’ACA en Ontario, le conseil de l’Ordre des psychologues est prêt à intégrer la réglementation de l’ACA dans sa structure de gouvernance.
Le 19 septembre 2019, l’Ordre a reçu une lettre de Todd Smith, ministre des Services à l’enfance et des Services sociaux et communautaires, et de Christine Elliott, ministre de la Santé, l’invitant à confirmer que la réglementation de l’ACA dans le cadre de sa structure de gouvernance l’intéresse. Les deux ministres précisent dans cette lettre que le renforcement de la surveillance des cliniciens du comportement protègera les Ontariennes et les Ontariens vulnérables contre le risque de préjudice et établira les attentes qui seront énoncées dans les normes professionnelles et les exigences en matière d’études auxquelles devront satisfaire les fournisseurs d’ACA de l’Ontario. La réglementation aidera également les familles à trouver des fournisseurs qualifiés et, au besoin, à porter plainte contre des fournisseurs. Les deux ministres ont ajouté qu’ils aimeraient commencer par réglementer les personnes qui assumeront un rôle de supervision, et qu’ils entrevoient élargir cette démarche pour inclure, avec le temps, la réglementation des cliniciens de première ligne.
Le 27 septembre 2019, le conseil de l’Ordre des psychologues a adopté une motion confirmant qu’il offrait de réglementer l’ACA à l’intérieur de sa structure de gouvernance.
Le 20 juillet 2023, le gouvernement de l’Ontario a approuvé les règlements pris en application de la Loi de 2021 sur la psychologie et l’analyse comportementale appliquée qui se rapportent à l’analyse comportementale appliquée (ACA). Le 1er juillet 2024, la Loi sera proclamée en vigueur et l’Ordre changera de nom pour devenir l’« Ordre des psychologues et des analystes du comportement de l’Ontario ». À compter du 1er juillet 2024, seuls les analystes du comportement inscrits à l’Ordre des psychologues et des analystes du comportement de l’Ontario seront autorisés à employer le titre d’« analyste du comportement » en Ontario.
À l’heure actuelle, l’Ordre travaille activement à la rédaction des règlements d’application de la nouvelle Loi et apporte les modifications nécessaires à ses règlements administratifs et ses politiques afin de réglementer les analystes du comportement. Ce travail doit être terminé avant que le gouvernement ne proclame la Loi dans sa totalité. La nouvelle Loi et les autres modifications législatives entreront en vigueur le 1er juillet 2024.
Les personnes qui désirent utiliser le titre d’« analyste du comportement » ou une variante, une abréviation ou un équivalent dans une autre langue de ce titre devront être inscrites à l’Ordre. Cette exigence s’applique aux superviseurs cliniques qui orientent et supervisent les activités d’ACA telles que l’évaluation du comportement, la conception d’un plan d’intervention, la mise en œuvre des plans d’intervention et la surveillance et l’évaluation des plans. À compter du 1er juillet 2024, seules les personnes inscrites à l’Ordre seront autorisées à employer le titre réservé d’« analyste du comportement ».
Les fournisseurs de services qui font des interventions d’ACA directement à des clients ou des aidants et qui relèvent d’un superviseur clinique en analyse comportementale ne seront pas réglementés.
La préinscription à titre d’analyste du comportement commencera normalement à le printemps 2024. Les analystes du comportement qui pratiquent l’ACA et satisfont aux exigences de l’inscription pourront alors faire une demande d’inscription à l’Ordre. La période de préinscription a pour but de permettre aux analystes du comportement qualifiés de continuer d’exercer et de fournir des services à leurs clients jusqu’à la date de proclamation de la Loi et au-delà de cette date, et d’ainsi assurer la continuité des soins. Pendant la période de préinscription, l’Ordre n’acceptera pas les demandes d’inscription des personnes qui exercent sous supervision.
Pour obtenir plus d’informations, visitez le Portail de l’analyse comportementale appliquée sur le site de l’Ordre des psychologues de l’Ontario, visualisez la nouvelle vidéo de la session d’information sur la réglementation de l’ACA, consultez la page FAQ pour obtenir des réponses aux questions fréquentes ou communiquez avec l’Ordre à aba@cpo.on.ca.
L’ajout de la profession d’analyste du comportement à l’Ordre aura peu ou pas d’effet pour la plupart des membres actuels. L’Ordre réglementera les deux professions séparément, de sorte que les interactions des psychologues et des associés en psychologie avec l’Ordre concernant leur pratique ou les attentes de l’Ordre ne devraient pas changer.
Les analystes du comportement auront leurs propres normes d’exercice, leur propre programme d’assurance de la qualité et des exigences d’inscription établies spécifiquement pour eux. Le Règlement sur la faute professionnelle et le Règlement sur l’assurance de la qualité seront révisés afin de s’appliquer à la fois à l’exercice de l’analyse comportementale appliquée et à l’exercice de la psychologie. Le conseil et les comités de l’Ordre seront élargis et se composeront de psychologues, d’associés en psychologie, d’analystes du comportement et de membres du public nommés par le gouvernement. Les décisions prises par les comités statutaires de l’Ordre seront fonction de l’expertise des membres de chacune des deux professions et des membres du public qui siègent à ces comités.
Certains membres de l’Ordre voudront s’inscrire à l’Ordre à titre d’analystes du comportement afin de pouvoir employer le titre réservé d’« analyste du comportement ». Ces membres seront alors titulaires de deux certificats d’inscription : un certificat qui les autorisera à exercer la psychologie et un autre qui les autorisera à exercer l’analyse comportementale appliquée. Les membres titulaires de deux certificats d’inscription devront satisfaire aux exigences d’inscription et aux attentes établies par l’Ordre pour chacune des deux professions.
Il n’y a aucun rapport entre la réglementation des analystes du comportement et les mesures prises par l’Ordre pour cesser d’inscrire des candidats qui ont obtenu une maîtrise en psychologie. Toute activité visant à mettre fin à l’inscription des titulaires d’une maîtrise sera exécutée complètement à part des activités visant à commencer la réglementation des analystes du comportement.
Le champ d’exercice des analystes du comportement ou les activités qu’ils font lorsqu’ils fournissent des services à des clients ne sont pas des actes autorisés ou des activités restreintes. Ils relèvent, par conséquent, du domaine public. Si une personne n’est pas inscrite à l’Ordre, elle doit connaître les restrictions prévues par la Loi concernant la façon dont elle se représente quand elle fournit des services d’analyse du comportement.
Lorsque la Loi de 2021 sur la psychologie et l’analyse comportementale appliquée (la Loi) sera proclamée, le titre d’« analyste du comportement » sera réservé uniquement aux personnes inscrites à l’Ordre à titre d’analystes du comportement. Ces personnes pourront indiquer tout certificat qu’elles possèdent, tel que le certificat BCBA ou BCBA-D, afin d’aider le public à comprendre leurs qualifications de fournisseurs de services de santé réglementés inscrits à l’Ordre. Les personnes qui ne sont pas membres de l’Ordre et qui emploient le titre d’« analyste du comportement » ou prétendent avoir un certificat ou une désignation montrant qu’elles ont les qualifications voulues pour exercer à titre d’analystes du comportement commettront une infraction à la Loi.
Les actes autorisés sont des activités ou des interventions en santé considérées comme pouvant causer des préjudices si elles sont accomplies par des personnes non qualifiées. On pense, par exemple, à l’administration d’une substance par injection, à l’immobilisation plâtrée de fractures, à la prescription de lunettes, à l’exécution d’une intervention chirurgicale, à la gestion de la naissance d’un enfant et à l’application d’une forme d’énergie. La liste complète des 14 actes autorisés se trouve à l’article 27, paragraphe 2, de la Loi de 1991 sur les professions de la santé réglementées (LPSR).
Étant donné le risque de préjudice qu’ils posent, les actes autorisés peuvent être accomplis seulement par des professionnels de la santé réglementés qui sont autorisés par la loi à le faire. La loi ne permet pas à toutes les professions de la santé d’exécuter des actes autorisés. Chaque profession de la santé est assujettie à une loi précisant, le cas échéant, les actes autorisés que ses membres ont le droit d’accomplir, par exemple, la Loi de 1991 sur les médecins, la Loi de 1991 sur les pharmaciens, la Loi de 1991 sur les psychologues ou la Loi de 1991 sur les infirmières et infirmiers, pour n’en nommer que quelques-unes.
Non. Les analystes du comportement ne pourront accomplir aucun des actes autorisés décrits dans la Loi. Un acte autorisé peut être accompli seulement par les membres des professions de la santé autorisés à le faire par la Loi de 1991 sur les professions de la santé réglementées (LPSR) et par la loi qui régit leur profession. La liste des 14 actes autorisés se trouve à l’article 27 de la LPSR. Cette interdiction s’applique actuellement aux personnes qui pratiquent l’analyse comportementale appliquée ou toute autre forme de thérapie comportementale et restera en place après la proclamation de la nouvelle Loi.
Si une personne inscrite à l’Ordre à titre d’analyste du comportement est également inscrite à un autre ordre de réglementation, et si son inscription à cet autre ordre lui permet d’accomplir un ou plusieurs actes autorisés, elle peut continuer d’accomplir l’acte ou les actes autorisés par la Loi ou par la loi régissant sa profession pendant qu’elle exerce cette autre profession.
De nombreux professionnels inscrits à d’autres ordres de réglementation, comme les infirmières et infirmiers, les travailleurs sociaux, les ergothérapeutes, les orthophonistes et les éducateurs, utilisent des techniques comportementales dans leur travail. Comme nous l’avons déjà mentionné, ces activités relèvent du domaine public et ne sont pas des activités restreintes. Par ailleurs, les professionnels désireux de se représenter comme des « analystes du comportement » ou comme des personnes qualifiées pour pratiquer l’analyse comportementale appliquée seront tenus de s’inscrire, en plus, à l’Ordre des psychologues et des analystes du comportement de l’Ontario.
Tous les professionnels de la santé sont tenus d’avoir une assurance de la responsabilité professionnelle. Les analystes du comportement devront, eux aussi, détenir cette assurance ou être couverts par une telle assurance dans tous les milieux où ils exercent. L’assurance doit être en place au moment de l’inscription et être confirmée tous les ans à l’Ordre lors du renouvellement de l’adhésion.
Les analystes du comportement qui sont employés par un organisme peuvent être couverts par l’assurance de la responsabilité professionnelle de leur employeur, à condition que cette assurance satisfasse aux exigences minimales établies par l’Ordre. Il est toutefois important de savoir que l’assurance de l’employeur couvre uniquement les services fournis dans le cadre du travail effectué pour cet employeur. Les analystes du comportement qui ont emploi et qui fournissent également des services à des clients en dehors de leur travail pour leur employeur ont l’obligation de souscrire, en plus, une assurance de la responsabilité professionnelle pour eux-mêmes.
Vous pouvez souscrire une assurance de la responsabilité professionnelle auprès d’associations, de sociétés d’assurances et d’autres organismes. La couverture d’assurance doit être conforme aux règlements administratifs de l’Ordre.
L’Ordre a créé un outil d’autosélection pour aider les personnes qui font de l’analyse comportementale, de la thérapie ou de l’intervention à déterminer si elles doivent s’inscrire à l’Ordre lorsque la période de préinscription commencera. Pour accéder à l’outil l’autosélection, cliquez ici.
Les parcours transitoires temporaires menant à l’inscription à l’Ordre prendront fin le 30 juin 2026 à 23 h 59.
Nous encourageons les personnes qui suivent actuellement la formation pour obtenir le certificat BCBA ou BCBA-D du Behavior Analyst Certification Board à terminer leur formation et à faire une demande d’inscription à l’Ordre en suivant le parcours transitoire #1. Les parcours transitoires prendront fin le 30 juin 2026 à 23 h 59.
Les attestataires doivent remplir le formulaire d’attestation de l’Ordre. Ce formulaire pourra être téléchargé à partir du portail de demande d’inscription ou du site Web de l’Ordre à la section « Ressources ».
On rappelle aux demandeurs que l’attestation doit provenir d’un attestataire approprié, c’est-à-dire d’une personne qui :
- possède l’une ou l’autre des qualifications professionnelles suivantes : analyste du comportement certifié par le Behaviour Analyst Certification Board (BCBA ou BCBA-D), ou psychologue ou associé en psychologie inscrit à l’Ordre des psychologues de l’Ontario et possédant une expertise dans l’analyse comportementale, et
- a observé le demandeur dans sa pratique et peut attester que le demandeur possède actuellement l’expérience et la compétence nécessaires pour exercer ses activités dans le champ d’exercice de la profession, ce qui inclut la prise de décisions cliniques.
Les psychologues et les associés en psychologie qui veulent pouvoir employer le titre réservé d’« analyste du comportement » doivent satisfaire aux exigences d’inscription établies pour obtenir un deuxième certificat d’inscription qui les autorise à pratiquer l’analyse comportementale.
De l’avis de l’Ordre, les titulaires de ces deux certificats n’ont pas fait les études requises en analyse comportementale, c’est-à-dire au niveau de la maîtrise ou des cycles supérieurs, pour s’inscrire à l’Ordre lors de leur entrée dans la profession ou en utilisant le parcours transitoire #2. De plus, les personnes qui font une demande d’inscription par le biais du parcours transitoire #2 doivent fournir la preuve qu’elles ont la compétence voulue pour effectuer de l’analyse comportementale en pratique autonome et prendre des décisions cliniques au sujet du soin des clients. Selon le Behavior Applied Certification Board, les titulaires d’un certificat RBT ou BCaBA doivent exercer sous supervision lorsqu’ils fournissent des soins à des clients et, par conséquent, ils ne peuvent pas s’inscrire à l’Ordre à titre d’analystes du comportement en suivant le parcours transitoire #2.
Chaque titulaire d’un certificat BCBA doit décider de maintenir, ou non, sa certification. Seules les personnes inscrites à l’Ordre à titre d’analystes du comportement pourront employer le titre de BCBA en Ontario. La certification BACB est nécessaire pour s’inscrire dans la plupart des états américains où l’analyse comportementale appliquée est réglementée, si bien que cette certification offre aussi la possibilité de travailler aux États-Unis.
Le Behavior Analyst Certification Board a récemment annoncé qu’à compter du 1er juillet 2026, les résidents de l’Ontario ne pourront plus faire de demande pour obtenir la certification BCBA ou passer l’examen. Les personnes ayant la certification BCBA et BCBA-D pourront cependant maintenir leur certification après le 1er juillet 2026.
À partir du jour de la proclamation de la nouvelle Loi, seules les personnes inscrites à l’Ordre pourront employer le titre réservé d’« analyse du comportement ». Comme le titre de BCBA inclut le titre d’« analyste du comportement », l’emploi du titre de BCaBA sera interdit en Ontario après la proclamation de la Loi.
Le Behavior Analyst Certification Board a récemment annoncé qu’à compter du 1er juillet 2024, il accordera le statut inactif volontaire aux certificats RBT et BCaBA des titulaires de l’Ontario. Pour obtenir plus de renseignements sur ce changement, veuillez communiquer directement avec le Behavior Analyst Certification Board.
La Loi de 1991 sur les professions de la santé réglementées (LPSR) stipule que le titre de « docteur » est un titre réservé en Ontario. À l’exception des chiropraticiens, des optométristes, des médecins, des psychologues et des dentistes, « nul ne doit employer le titre de « docteur », une variante ou une abréviation, ou un équivalent dans une autre langue, lorsqu’il donne ou propose de donner, en Ontario, des soins médicaux à des particuliers. » (par. 33 (1), LPSR).
Les analystes du comportement inscrits ne seront pas autorisés à employer le titre de « docteur », une variante ou une abréviation de ce titre lorsqu’ils fourniront ou proposeront de fournir des services d’analyse comportementale appliquée.
Seuls les analystes du comportement ayant un certificat d’inscription de l’Ordre autorisant l’exercice autonome peuvent fournir de la supervision clinique à des analystes du comportement exerçant sous supervision.
Les personnes désireuses de s’inscrire à l’Ordre à titre d’analystes du comportement devront se soumettre à une vérification de l’aptitude à travailler auprès de personnes vulnérables. Les demandeurs qui vivent dans les régions qui ne font pas de telles vérifications aux fins de l’inscription devront fournir une vérification du casier judiciaire et d’affaires judiciaires de niveau 2. Ces demandeurs devront également signer un engagement et une entente avec l’Ordre.
La vérification de l’aptitude à travailler auprès de personnes vulnérables est le type de vérification policière standard auquel doivent se soumettre les individus travaillant avec des personnes vulnérables. Ce type de vérification permet de recueillir des informations commises par les demandeurs, y compris les condamnations, les mandats non exécutés, les ordonnances judiciaires, les accusations et les suspensions du casier judiciaire (réhabilitations) en raison d’infractions sexuelles.
Tous les demandeurs d’inscription à l’Ordre à titre d’analystes du comportement doivent inclure les résultats d’une vérification de l’aptitude à travailler auprès de personnes vulnérables dans leur dossier de demande d’inscription. L’analyse comportementale appliquée est souvent utilisée pour traiter l’autisme et d’autres déficiences développementales, et les analystes du comportement travaillent étroitement avec des enfants et d’autres personnes vulnérables dont ils ont le soin et sur lesquels ils exercent une autorité. La vérification de l’aptitude à travailler auprès de personnes vulnérables offre une protection supplémentaire au public parce qu’elle permet d’obtenir d’un organisme extérieur des renseignements sur la moralité des demandeurs.
Seules les vérifications de l’aptitude à travailler auprès de personnes vulnérables qui ont été effectuées dans les six (6) mois précédant la date à laquelle l’Ordre les reçoit seront acceptées.
Pour obtenir une vérification de l’aptitude à travailler auprès de personnes vulnérables, veuillez communiquer avec votre service policier local pour obtenir plus de renseignements. Vous avez la responsabilité d’obtenir le type exact de vérification et d’assumer tous les frais s’y rattachant. Les délais de traitement varient d’un service policier à l’autre et l’obtention des résultats peut prendre un certain temps. Nous vous recommandons de vous donner suffisamment de temps pour faire une demande de vérification de l’aptitude à travailler auprès de personnes vulnérables, mais pas plus de six mois avant la date de votre demande d’inscription.
Tous les demandeurs d’inscription doivent utiliser le portail d’inscription de l’Ordre pour téléverser les résultats originaux de la vérification de l’aptitude à travailler auprès de personnes vulnérables. Les demandeurs devraient conserver une copie scannée des résultats de la vérification dans leurs dossiers. Si le service policier vous a fourni les résultats originaux sur papier, veuillez les fournir à l’Ordre avec une lettre d’accompagnement.
Les demandeurs vivant à Toronto doivent s’adresser au service policier de Toronto pour obtenir une vérification de l’aptitude à travailler auprès de personnes vulnérables. Le service policier de Toronto vous permet d’obtenir la vérification en ligne, en personne ou par la poste. Consultez le site Web du service policier de Toronto pour obtenir plus d’informations.
Le service policier de Toronto a attribué à l’Ordre un code d’organisme/numéro de programme (« Agency Code/Program Number ») unique que vous devrez fournir. Voici le code : 202311TPSONA3383.
Si vous vivez actuellement à l’extérieur du Canada et qu’il vous est impossible d’obtenir une vérification de l’aptitude à travailler auprès de personnes vulnérables, veuillez communiquer avec l’Ordre à aba@cpo.on.ca.
L’Ordre tient un tableau consultable de tous ses membres actuels. À compter du 1er juillet 2024, le tableau renfermera des informations sur les analystes du comportement inscrits. Vous pouvez aussi vous adresser à l’Ordre par téléphone au 416-961-8817 ou par courriel à cpo@cpo.on.ca.
Oui. L’Ordre mènera une enquête si vous avez des préoccupations au sujet de services qui vous ont été fournis sous la supervision d’un analyste du comportement. Sachez toutefois que l’enquête portera sur le membre de l’Ordre et non pas sur la personne supervisée. Le membre de l’Ordre qui supervise est responsable des services d’analyse comportementale fournis sous supervision.
L’Ordre fera également enquête sur l’emploi incorrect des titres de « docteur », d’« analyste du comportement » et de toute variante de ces titres réservés. L’Ordre mènera également enquête sur les personnes qui ne sont pas inscrites à l’Ordre et qui se représentent comme étant qualifiées pour exercer à titre d’analystes du comportement.
No. The hallmark of self-regulation is a professional’s ability to independently reflect and make ethical decisions in the best interest of their clients. This self-awareness is relevant to practicing within one’s competence, which requires knowledge, skill, and clinical judgment. Registration as a Behaviour Analyst does not imply that one can practice with any client, in any situation, and for any purpose within the scope of applied behaviour analysis. One must know what they know, but as importantly, they must know that they don’t know everything. Awareness of limits of professional competence and taking disciplined steps to practice safely is required of all registrants of the College as indicated by the Standard of Professional Conduct (2017) which states:
5.1 Practising Within Areas of Competence
Members may only provide services within their authorized areas of practice and with their authorized client populations, and then only when competent to provide those particular services.
Members wishing to provide services that are beyond their competence but are within their authorized areas of practice and with their authorized client populations may only do so under the professional guidance of a member who is authorized and competent to provide the services being delivered.
Comment devenir membre de l’Ordre
Applicants should review the College’s Registration Guidelines prior to making an application for registration. The College also has Flowcharts which illustrate the different registration pathways:
- Registration Flowchart: Psychologist – Educated in Canada or the USA
- Registration Flowchart: Psychological Associate – Educated in Canada or the USA
- Registration Flowchart: Psychologist – Educated Outside Canada or the USA
- Registration Flowchart: Psychological Associate – Educated Outside Canada or the USA
Guidelines can be found here:
- Registration Guidelines: Psychologist – Supervised Practice
- Registration Guidelines: Psychological Associate – Supervised Practice
If you are unsure about which application route is applicable for you take our How to Apply quiz here.
There isn’t a deadline for receipt of Supervised Practice or Interim Autonomous Practice applications. Applications are reviewed on an on-going basis throughout the year. Once the College has received your completed application form, the application fee, and all supporting documentation, your application is ready for review. The review process is usually completed in four to six weeks.
Aussitôt que l’Ordre reçoit le formulaire de demande d’inscription, les frais d’inscription et tous les documents justificatifs, votre demande est considérée comme étant & #171; prête à étudier » et l’étude de votre dossier commence. Lorsque votre demande est « prête à étudier », il faut de quatre à six semaines pour la traiter. Quand l’étude de votre demande est terminée, l’Ordre vous envoie une lettre par la poste confirmant le résultat.
Si le registrateur n’a pas la certitude que vous remplissez les exigences en matière d’études ou de bonnes mœurs, ou s’il doute que vous ayez la formation voulue pour travailler dans le(s) domaine(s) d’exercice que vous proposez, votre demande est renvoyée au comité d’inscription pour une étude plus poussée. Dans ce cas, une lettre vous est envoyée pour vous informer du renvoi de votre dossier au comité d’inscription, et vous avez un délai d’au moins 30 jours pour soumettre tout renseignement supplémentaire qui aidera le comité d’inscription dans son étude. Au cours de l’année, le comité d’inscription se réunit environ toutes les six semaines. L’étude de votre dossier par ce comité se fait lors de sa réunion suivant le délai d’avis de 30 jours.
Nous encourageons les candidats à présenter leur demande d’inscription dûment remplie accompagnée de tous les documents justificatifs le plus tôt possible. Les candidats ont la responsabilité de vérifier si l’Ordre a bien reçu tous leurs documents. Ils peuvent communiquer avec le personnel de l’Ordre par téléphone ou par courriel pour savoir où en est leur demande.
Lorsque l’Ordre reçoit des documents justificatifs avant la demande d’inscription, il verse ces documents justificatifs dans un dossier portant votre nom. Lorsque qu’il reçoit la demande d’inscription, il la verse dans le dossier qui renferme déjà les documents justificatifs.
Les candidats ont 24 mois, à compter de la date de réception de leur demande d’inscription, pour présenter les documents justificatifs nécessaires à la délivrance de leur certificat d’inscription. Toute demande d’inscription qui n’a pas donné lieu à la délivrance d’un certificat d’inscription ou à une confirmation d’admissibilité expire automatiquement 24 mois après la date à laquelle elle a été reçue par l’Ordre. La demande d’inscription et tous les documents justificatifs sont alors détruits. Les frais d’inscription ne sont pas remboursables.
Dans le cas des candidats qui ont terminé les études exigées pour obtenir un grade mais qui n’ont pas encore obtenu leur grade comme tel, l’Ordre accepte le relevé de note pré-collation des grades afin d’étudier leur demande d’inscription. Le relevé de notes doit toutefois être accompagné d’une lettre signée par le sénat ou le registraire de l’université ou par un mandataire approprié du département de psychologie, comme le directeur de la formation clinique, et cette lettre doit confirmer la date à laquelle le candidat a terminé avec succès toutes les exigences en matière d’études. La letter doit être soumise a l’Ordre directement à partir de l’Université ; l’Ordre n’acceptera pas une copie d’etudiante de la letter.
Non. L’Ordre accepte seulement les relevés de notes qui lui sont envoyés directement par une université. Les candidats ont la responsabilité de communiquer avec leur université et de lui demander d’envoyer une copie de leur relevé de notes officiel à l’Ordre.
La date du début du travail supervisé approuvée par l’Ordre est la date à laquelle votre superviseur principal et votre superviseur suppléant confirment tous les deux qu’ils ont commencé à superviser votre travail, ou la date à laquelle l’Ordre a reçu le dernier document justificatif faisant partie de votre demande d’inscription, la date la plus tardive étant retenue.
Non. Vous pouvez faire une demande pour exercer sous supervision même si vous ne travaillez pas encore en Ontario. Envoyez à l’Ordre la demande d’inscription au complet, accompagnée des frais d’inscription et des documents justificatifs, mais ne remplissez pas la section « Exercice sous supervision autorisé & #187; du formulaire de demande ni les formulaires de consentement du superviseur principal et du superviseur suppléant. L’Ordre procèdera à l’évaluation de vos attestations d’études. Si votre demande est jugée acceptable, le registrateur attendra que vous ayez trouvé un milieu de travail convenable et que vous ayez nommé deux superviseurs pour délivrer votre certificat d’inscription. En attendant, si votre demande d’inscription est approuvée, vous pouvez choisir de passer l’examen EPPP et l’examen de jurisprudence et d’éthique.
Yes. Supervised practice is intended to prepare you to practice psychology in Ontario. It must be completed here under the College’s Standards of Professional Conduct and Ontario legislation. The College’s mandate is to protect the public of Ontario. Psychological services provided in another province or state follow the rules of the regulatory board for psychology in that province or state only.
Les candidats ont la responsabilité de trouver eux-mêmes un emploi acceptable ainsi qu’un superviseur principal et un superviseur suppléant. En général, lorsque vous trouvez un emploi, votre employeur a au moins un membre de l’Ordre qui travaille sur place ou qui peut conseiller à l’organisme une personne capable de superviser votre travail. L’Ordre a un tableau public en ligne, à www.cpo.on.ca, qui peut vous aider dans votre recherche de superviseurs. L’Ontario Psychological Association, www.psych.on.ca, a aussi une liste des membres de l’Ordre qui sont disponibles pour faire de la supervision.
L’Ordre accepte seulement les paiements effectués par carte de crédit.
No, please use the online application.
You may receive a copy of all information and each document that the College has that is relevant to your application. Please note that the College does not return original documents however, you may ask for a copy of the documents in your registration file.
To obtain a copy of your registration file you must makea written request to the College either in-person, by mail, or by e-mail. There is a charge of 20¢ per page for this. Upon receiving the written request, registration staff will determine the number of pages in the record and advise you of the cost before proceeding.
Oui. Vous pouvez faire une demande d’inscription à titre d’associé en psychologie (exercice supervisé) et joindre à votre demande tous les documents justificatifs exigés et les frais d’inscription, mais ne remplissez pas la section du formulaire de demande intitulée « Exercice sous supervision autorisé » ni les formulaires de consentement du superviseur principal et du superviseur suppléant. L’Ordre examinera vos attestations d’études mais attendra que vous ayez terminé votre expérience de travail post-maîtrise pour étudier votre demande d’inscription.
En attendant, si vos attestations d’études sont approuvées, vous pouvez passer l’Examen de Pratique Professionnelle en Psychologie (EPPP) et l’examen Jurisprudence and Ethics Examination (JEE).
Pour inclure les familles dans votre Déclaration de compétence, vous devez effectuer l’évaluation des familles et intervenir auprès d’elles pendant votre période d’exercice sous supervision. Dans ces cas, les familles sont votre groupe client primaire. Si vous ne fournissez pas de service directement aux familles, il n’est pas approprié d’indiquer les familles dans votre Déclaration de compétence même si vous voyez les parents ou les familles dans le contexte de votre travail avec les enfants ou les adolescents qui font partie des familles. L’Ordre reconnaît que lorsque les enfants et les adolescents sont votre groupe client déclaré, vous devez souvent rencontrer les parents ou les familles. Il est important de faire la distinction entre les familles comme groupe client particulier avec qui vous travaillez, et la participation des familles dans le contexte du travail que vous faites avec les enfants et les adolescents qui font partie des familles.
Should you have any questions or concerns about a Registration Committee decision, you may contact the College directly to speak with a Registration Assistant, or you may e-mail the College at registration@cpo.on.ca
If you disagree with a decision of the Registration Committee you have the right to appeal the decision to the Health Professions Appeal and Review Board (HPARB).
You must write directly to HPARB within 30 days of receiving the Registration Committee’s decision letter.
HPARB may be contacted at the address below:
Health Professions Appeal and Review Board
151 Bloor Street West, 9th Floor
Toronto, ON, M5S 1S4
Telephone: 416-327-8512
Toll Free: 1-866-282-2179
TTY/TDD: 416-326-7TTY or 416-326-7889 1-877-301-0TTY or 1-877-301-0889
Fax: 416-327-8524
E-mail: hparb@ontario.ca
Website: www.hparb.on.ca
O.Reg 74/15 - Registration
The new regulation (O. Reg. 74/15) replaces O. Reg. 533/98 and revises and updates the requirements for registration with the College. The new regulation reflects changes that were approved by Council and submitted to the Ontario government for approval in October 2013.
The revised Registration Regulation became effective on April 7, 2015.
The most significant changes are that:
- The new regulation is more specific about the graduate psychology training requirements for registration as a Psychologist and as a Psychological Associate. Whereas the old regulation indicated that an applicant had to have completed a degree from “a program of study with content that is primarily psychological in nature as required in the guidelines published by the College”, the new regulation indicates that a Psychologist applicant must have a doctoral degree from a CPA-accredited or equivalent psychology program. The specific curriculum content of acceptable psychology programs for master’s level Psychological Associate registration is also now outlined in the regulation.
- Other requirements previously outlined in the guidelines, such as those regarding supervised practice, are now specified in the regulation.
- The examinations (EPPP, JEE, and Oral Exam) applicants must pass as a requirement of registration are now specified in the regulation.
- The new regulation eliminates the “status” of certificates for Inactive, Retired, and Academic registration; these will now become classes of certificates of registration. This does not change the conditions for holding these certificates.
- Any applicant whose completed application to the College is received on or after April 7, 2015, will need to meet the requirements as outlined in the new regulation.
- Applicants who applied and whose required documentation to complete their application for review by the College had been received by the College prior to April 7, 2015, will be processed under the previous (old) regulation
- Applicants who applied and whose required documentation to complete their application for review by the College had not been received prior to April 7, 2015, will be notified that once they complete their application it will be processed under the new regulation.
Yes – such applicants will now be required to pass the College’s Jurisprudence and Ethics Examination (JEE) as a requirement for obtaining a Certificate for Autonomous Practice. Qualified applicants will initially be able to register for and hold a Certificate for Interim Autonomous Practice for up to 12 months, which will enable them to practise while they prepare for and write the JEE.
For more information, please feel free to contact the College at cpo@cpo.on.ca if have any questions
Examens d'inscription
Lorsque votre demande d’inscription à l’Ordre est approuvée, l’Ordre vous donne tous les détails nécessaires pour vous inscrire à l’examen EPPP et à l’examen de jurisprudence et d’éthique. Vous n’avez pas besoin d’être titulaire d’un certificat vous autorisant à exercer sous supervision pour passer ces deux examens, mais votre demande d’inscription doit avoir été approuvée par l’Ordre.
L’examen EPPP est un examen informatisé à choix multiples que l’on peut passer tout au long de l’année à divers centres désignés d’examens informatisés partout au Canada et aux États-Unis.
L’examen de jurisprudence et d’éthique est un examen écrit à choix multiples administré à plusieurs endroits en Ontario deux fois par année, au printemps et à l’automne. Les dates du prochain examen sont affichées sur le site Web de l’Ordre à www.cpo.on.ca.
Les membres qui exercent sous supervision doivent, pour rester en règle, passer l’examen EPPP et l’examen de jurisprudence et d’éthique dans l’année suivant l’obtention du certificat les autorisant à exercer sous supervision.
Vous pouvez passer l’examen EPPP et l’examen de jurisprudence et d’éthique dans l’ordre que vous préférez.
L’examen oral représente la dernière étape du processus d’inscription à l’Ordre. Pour être invité à passer un examen oral, vous devez avoir réussi à l’examen EPPP et à l’examen de jurisprudence et d’éthique et avoir satisfait à toutes les autres exigences établies, y compris celle de la période d’exercice sous supervision autorisé.
Non. Le personnel de l’Ordre n’est pas autorisé à donner les résultats des examens par téléphone, par télécopieur ou par courriel. Les résultats des examens sont envoyés aux candidats par la poste. Les résultats de l’examen de jurisprudence et d’éthique sont envoyés par la poste environ 6 semaines après la date de l’examen, et les résultats de l’examen EPPP sont envoyés par la poste environ 4 semaines après la date de l’examen. Si vous vous demandez pourquoi vous n’avez pas encore reçu vos résultats d’examen, communiquez avec l’Ordre pour demander s’ils ont été mis à la poste.
Lorsque votre demande d’inscription à l’Ordre est approuvée, l’Ordre vous donne tous les détails nécessaires pour vous inscrire à ces deux examens.
L’Ordre ne recommande aucune méthode particulière pour vous préparer à l’examen EPPP. Certaines personnes trouvent utile le matériel commercial de préparation à des examens publié par certaines compagnies, mais l’Ordre ne cautionne pas ce matériel. Pour savoir comment vous préparer à l’examen EPPP, y compris un examen informatisé, allez sur le site Web de l’Association of State and Provincial Psychology Boards (ASPPB) à www.asppb.net.
Applicants who took the EPPP as part of the registration/licensure requirements in another jurisdiction, and who received a scaled score of at least 500 or a percentage score of at least 70% are not required to re-take this examination.
Please arrange to have your EPPP results forwarded directly to the College of Psychologists of Ontario by contacting the Association of State and Provincial Psychology Boards (ASPPB) at the following link: http://www.asppb.net/?page=ScoreTransfer
The College recommends that candidates review the preparatory information outlined in the document titled Preparing to take the Jurisprudence and Ethics Examination.
As well as the list of relevant Legislation and Standards
Additionally, detailed information about the JEE including (but not limited to) an Examination Blueprint of the content of the examination, pass point and scoring, number of attempts permitted, and exam accommodations is outlined in the Examinations section of the Registration Guidelines: Supervised Practice:
Psychological Associates’ Exams
The Supervision Resource Manual also includes some information on how candidates can prepare to take the JEE.
Candidates generally perform very well on the JEE. Ontario-educated candidates tend to do better than those candidates who did not receive their education in Ontario.
The pass rate on the JEE over the past 11 years has been 89%. Only 6% of candidates have scored under 60%. The cut-score is generally about 66%, ranging from 62% to 69% for any one particular administration of the JEE. The highest score on each individual exam ranges from 86% to 98% and the lowest score ranges from 35% to 65%. The average score for the JEE over the past 11 years is 76%.
Of particular note is that the pass rate observed on the JEE, both for Ontario educated and internationally educated candidates, is comparable to that of other high stakes professional licensing examinations.
Internationally educated candidates are a very diverse group from many different countries. Many factors affect their success on the JEE, including language of education and language of clinical practice, years since graduation, and practice patterns in the country of education, that is, whether they are similar to Canada or different.
Familiarity with the exam format may also affect the pass rate. In other words, candidates who have experienced multiple-choice exams during their education program may perform better than those candidates who have not experienced multiple-choice exams.
The leading psychometric standard-setting body, the American Educational Research Association (AERA), specifically recommends that professional licensing examinations not use a “norm-reference approach” – that is, adjusting an examination’s pass rate so that a specified percentage of candidates pass each time. Standard 11.16 says
“The level of performance required for passing a credentialing test should depend on the knowledge and skills necessary for credential-worthy performance in the occupation or profession and should not be adjusted to control the number or proportion of persons passing the test.”
American Educational Research Association, American Psychological Association, National Council on Measurement in Education. (2014). Standards for educational and psychological testing. Washington DC: American Educational Research Association.
Vous pouvez vous attendre à recevoir le résultat de votre examen de jurisprudence et d’éthique (EJE) environ 6 semaines après avoir passé l’examen.
Il faut environ 1 à 2 semaines pour enregistrer et vérifier toutes les réponses des candidats. Le comité de l’examen de jurisprudence et d’éthique (comité de l’EJE) commence ensuite le processus d’analyse psychométrique des questions et d’établissement de la note de passage pour cet examen particulier. Les lignes directrices sur l’inscription décrivent la procédure suivie par le comité de l’EJE pour établir la note de passage. Ce processus prend environ d’une à deux semaines. Une fois la note de passage de l’examen établie et les résultats individuels vérifiés, le personnel de l’Ordre prépare l’avis écrit qui sera envoyé à chaque candidat, ce qui prend d’une à deux semaines.
Le personnel de l’Ordre n’est pas autorisé à donner les résultats de l’examen par téléphone, par télécopieur ou par courriel.
The College does not provide feedback regarding a candidate’s performance within specific areas of the blueprint of the JEE or make recommendations for remediation. Only the total score that the candidate achieved is provided, along with the cut-score, mean, and standard deviation.
The JEE is a professional licensing exam. Professional licensing exams are used to evaluate knowledge, skills, and abilities (i.e. competence) required to practise a profession at an entry-level, in the interest of the protection of the public. These types of examinations are not designed or intended to provide feedback to candidates. In this case, the JEE is used to evaluate knowledge of jurisprudence, ethics, and standards related to the practice of psychology in Ontario.
The reliability of the results of any exam is strongly related to the number of items (questions) on the exam. Similarly, the reliability of any information provided to candidates related to scales within the exam is related to the number of items within that scale. Given the JEE Examination Blueprint (as outlined in the Registration Guidelines), some categories may have as few as four to seven items. When there is a small number of items in a scale the reliability and also validity of any report based on these scales would be questionable as feedback to the candidate.
The Registration Guidelines: Supervised Practice (psychologist) and Registration Guidelines: Supervised Practice (psychological associate), describe the oral examination, and the Supervision Resource Manual provides information on how candidates should prepare for the oral examination.
Candidates who have special requirements arising from documented impairments or disabilities may request accommodations in taking any of the College’s required examinations.
The College’s Examination Accommodation Policy is found in the Registration Guidelines, and the forms required for requesting an accommodation are found in the application for registration.
If you have a question about requesting an examination accommodation you may contact exams@cpo.on.ca for assistance.
The forms required for requesting an examination accommodation are found in either the application for supervised practice or the application for interim autonomous practice.
How to Apply
If you have a question about completing the examination accommodation forms you may contact exams@cpo.on.ca for assistance.
You may submit your request for an examination accommodation at the same time that you apply for registration with the College or you may submit your request later if necessary.
In all cases, the College’s examination accommodation request form, and documentation, either from your regulated health care professional or the university from which you graduated, must be submitted to the College at least 60 calendar days in advance of an examination administration in order to allow sufficient time for your request to be reviewed and for accommodations to be arranged.
Exam candidates requesting accommodation will be advised of the College’s decision within ten (10) business days of the submission date, unless more information is needed to effectively evaluate the accommodation request.
A candidate who has applied and has been granted examination accommodation for a permanent or long-term disability will not be required to re-apply for accommodation for subsequent attempts but must confirm to the College that accommodations are still required.
If the request was related to a temporary condition (e.g. recent injury or pregnancy-related conditions) or if five years have passed since the initial accommodation request, the College may request updated information confirming the continued need for accommodation.
When re-applying to take the JEE, the College’s JEE Registration Form will require you to indicate whether you need accommodations, and if so to indicate whether you have already submitted the necessary accommodation request form.
When re-applying to take the EPPP, the ASPPB’s candidate request form will require you to indicate whether you need accommodations.
If the accommodation that you require has changed in any way from what was previously granted, you may be required to re-apply. Please contact exams@cpo.on.ca for assistance.
Personnes formées à l'étranger ou aux États-Unis
Oui, vous pouvez commencer le processus d’inscription avant d’arriver au Canada. Les lignes directrices sur l’inscription expliquent les étapes du processus d’inscription que vous pouvez franchir avant de déménager au Canada.
Registration Guidelines: Registration Process – Psychologist
Registration Guidelines: Registration Process – Psychological Associate
Si vous avez obtenu votre grade à l’extérieur du Canada ou des États-Unis, vous devez le faire évaluer pour savoir s’il est comparable au même grade décerné par une université canadienne. Cette évaluation doit être effectuée par World Education Services (WES) (www.wes.org/ca) ou par Comparative Education Service (CES) (https://learn.utoronto.ca/comparative-education-service).
L’évaluation doit montrer que le grade le plus élevé que vous avez obtenu en psychologie est une maîtrise ou un doctorat. Même si le rapport de WES ou de CES indique à l’Ordre que vos attestations d’études sont comparables à la maîtrise ou au doctorat décerné par une université canadienne, l’Ordre se réserve le droit de prendre la décision finale à l’égard du grade que vous avez obtenu et déterminera, conformément aux lignes directrices, si le contenu de votre grade est principalement de nature psychologique.
Educated Outside of Canada/USA / Evaluation of Academic Credentials
Si votre relevé de notes et vos documents officiels de l’université sont établis dans une langue autre que le français ou l’anglais, vous devez prendre les mesures nécessaires pour les faire traduire par un traducteur officiel. Il incombe aux candidats d’assumer le coût de la traduction de leurs documents.
Si une université à l’extérieur du Canada ou des États-Unis ne peut pas envoyer un relevé de notes directement à l’Ordre, l’Ordre peut accepter une copie certifiée conforme du relevé de notes que l’université a remis au candidat.
Non. Vous pouvez faire une demande pour exercer sous supervision en présentant la demande d’inscription, les documents justificatifs requis et les frais d’inscription, mais ne remplissez pas la section « Exercice sous supervision autorisé » du formulaire de demande ni les formulaires de consentement du superviseur principal et du superviseur suppléant. L’Ordre examinera vos attestations d’études mais attendra que vous ayez trouvé un emploi acceptable et des superviseurs pour étudier votre demande d’inscription.
En attendant, si vos attestations d’études sont approuvées, vous pouvez passer l’Examen de Pratique Professionnelle en Psychologie (EPPP) et l’examen Jurisprudence and Ethics Examination (JEE).
Non. Vous pouvez acquérir l’expérience de travail post-maîtrise à l’extérieur de l’Ontario ou du Canada.
The steps in the registration process are outlined in detail in the Registration Guidelines, however, a flowchart illustrating the steps in the registration process for applicants whose degrees are from outside of Canada and USA is also available in the “Applicants” section of the College’s website. There is a flow chart for psychological associate applicants and a flow chart for psychologist applicants. You can find the flowcharts here:
Les candidats ont la responsabilité de trouver eux-mêmes un emploi acceptable ainsi qu’un superviseur principal et un superviseur suppléant. En général, lorsque vous trouvez un emploi, votre employeur a au moins un membre de l’Ordre qui travaille sur place ou qui peut conseiller à l’organisme une personne capable de superviser votre travail. L’Ordre a un tableau public en ligne, à www.cpo.on.ca, qui peut vous aider dans votre recherche de superviseurs. L’Ontario Psychological Association, www.psych.on.ca, a aussi une liste des membres de l’Ordre qui sont disponibles pour faire de la supervision.
You may receive a copy of all information and each document that the College has that is relevant to your application. Please note that the College does not return original documents however, you may ask for a copy of the documents in your registration file.
To obtain a copy of your registration file you must makea written request to the College either in-person, by mail, or by e-mail. There is a charge of 20¢ per page for this. Upon receiving the written request, registration staff will determine the number of pages in the record and advise you of the cost before proceeding.
Oui. Vous pouvez faire une demande d’inscription à titre d’associé en psychologie (exercice supervisé) et joindre à votre demande tous les documents justificatifs exigés et les frais d’inscription, mais ne remplissez pas la section du formulaire de demande intitulée « Exercice sous supervision autorisé » ni les formulaires de consentement du superviseur principal et du superviseur suppléant. L’Ordre examinera vos attestations d’études mais attendra que vous ayez terminé votre expérience de travail post-maîtrise pour étudier votre demande d’inscription.
En attendant, si vos attestations d’études sont approuvées, vous pouvez passer l’Examen de Pratique Professionnelle en Psychologie (EPPP) et l’examen Jurisprudence and Ethics Examination (JEE).
Préoccupations et plaintes - général
Complaints and reports are different ways of letting the College know about your concerns. There are several key differences between a complaint and a report:
| Investigation | Complaint / Reporter Involvement |
Timelines | Review | |
| Complaint | The ICRC must investigate every complaint it receives.* | The complainant:
|
150 days. The College can extend this timeline | The complainant and member may ask the Health Professions Review Board (HPARB) to review the ICRC’s decision. |
| Report | Not every report is investigated. The Registrar decides what to do with each report on a case-by-case basis | A report:
|
There is no set time for investigating a report. | HPARB cannot review the ICRC decision. |
Anyone who has a concern about a psychologist or psychological associate can file a complaint or submit a report. This includes a client, a family member, or friend of the client, an employer, an insurer, a colleague, or a general member of the public.
Clients do not have to make a complaint or report. However, some people, in some situations, do have to make a Mandatory Report. For more information, please click here.
You do not have to be involved in the College’s investigation. The College will still conduct a full investigation of your complaint and give you a copy of the decision.
Yes. Please see additional information about the College’s facilitated resolution process.
The College has a strict duty of confidentiality. It will not share your information with anyone outside of the ICRC investigation. However, on some occasions, the information may become public:
Referral to the Discipline Committee: Discipline hearings are public. However, the Discipline Committee can ban the publication of information that could identify you.
HPARB review: The College must give its investigation record to HPARB. HPARB also holds public hearings. HPARB is independent of the College and has its own processes. You may contact HPARB directly should you have any questions.
Complainants may find it helpful to have a lawyer, but it is not necessary. Most complainants proceed without a lawyer.
Members often do use lawyers when responding to complaints or reports. This is because the process may have a significant impact on the member’s practice and career.
The role of the College is to protect the public from harm. The College does so by setting and upholding rules and Standards for its members. These rules and Standards address many different concerns, including:
- Boundaries and sexual abuse;
- Appropriateness of services;
- Supervision;
- Fees and billing;
- Confidentiality and disclosure of information.
The College’s standards and rules cover most of the concerns brought to the College’s attention. Please contact the College if you are not sure whether your concerns are covered.
No. College staff can tell you whether the conduct you describe is covered by the College’s standards and rules. However, the staff could not tell you whether the member broke those rules. The ICRC will be able to decide whether it has concerns after an investigation.
No. The College cannot get involved in fee arrangements or make financial awards.
No. The College only has jurisdiction over individual members.
Le pouvoir de l’Ordre se limite à la conduite des psychologues et des associés en psychologie. Au besoin, toutefois, l’Ordre prend des mesures pour empêcher toute personne qui n’est pas membre de l’Ordre de faire ce qui suit :
- employer le titre de « psychologue » ou d’« associé en psychologie », en contravention de la Loi de 1991 sur les psychologues ;
- se faire passer pour une personne qui est qualifiée pour exercer la psychologie en Ontario à titre de « psychologue » ou d’« associé en psychologie », ou dans une spécialité de la psychologie, en contravention de la Loi de 1991 sur les psychologues ;
- employer le mot « psychologue » ou « associé en psychologie », une abréviation de ces mots ou un mot équivalent dans une autre langue pour décrire les services qu’elle offre ou qu’elle fournit, en contravention de la Loi de 1991 sur les psychologues ;
- accomplir l’acte autorisé de communiquer un diagnostic, en contravention de la Loi de 1991 sur les professions de la santé réglementées ;
- employer le titre de « docteur » lorsqu’elle fournit ou offre de fournir des services de santé, en contravention de la Loi de 1991 sur les professions de la santé réglementées.
The College will try to direct you to another body that may be able to address your concerns.
L’Ordre doit savoir qui est l’auteur d’une plainte pour faire enquête sur la plainte. L’Ordre a des procédures d’enquête qui sont conçues pour que tous les renseignements sur une plainte soient tenus confidentiels à l’intérieur de l’Ordre. Si un membre de l’Ordre ou un plaignant est insatisfait d’une décision rendue par le comité des demandes de renseignements, des plaintes et des rapports, il peut demander qu’un examen de la décision soit effectué par la Commission d’appel et de révision des professions de la santé (la « Commission » ). Dans ces cas, l’Ordre ne pas peut garantir que les renseignements demeureront confidentiels parce que la Commission est un organisme indépendant de l’Ordre et que ses examens sont ouverts au public.
Si, après une enquête sur une plainte, les allégations sont renvoyées au comité de discipline, l’affaire fera l’objet d’une audience ouverte au public. L’Ordre fait tout son possible pour que le comité de discipline interdise la publication des renseignements sur les services psychologiques qui ont donné lieu à la plainte.
Si vous craignez qu’on vous identifie lorsque vous déposez une plainte, nous vous encourageons à appeler l’Ordre et à discuter de vos craintes avec le personnel chargé des enquêtes. Vous n’avez pas besoin de vous identifier lorsque vous faites cet appel.
No, there is no time limit for filing a complaint. However, the College recommends that you raise your concerns as soon as possible. The earlier a complaint or report is received, the fewer problems may arise with the investigation. For example, it is more likely that relevant documents will still exist and witnesses can be located.
Mandatory reports have specific timelines attached. Please see the FAQs about mandatory reports.
Non. Tous les renseignements fournis à l’Ordre doivent être remis au comité des demandes de renseignements, des plaintes et des rapports.
L’Ordre est autorisé à prendre des mesures qui ont pour but de protéger le public et qui portent sur la conduite éthique, la compétence ou la capacité future d’un de ses membres. L’Ordre ne peut toutefois pas intervenir dans un litige d’ordre financier concernant des honoraires, ou exiger qu’un membre change d’opinion ou qu’il modifie un rapport.
Préoccupations et plaintes – deposer une plainte ou un rapport
You can submit a complaint or report to the College through electronic forms. You may also submit a complaint or report in writing or other recorded format, including film and audio. These can be sent directly to the College by email, fax, or regular mail.
You should provide as many details about your concerns as possible. Supporting documents such as emails, reports or bills are also helpful. You may also provide the names of relevant witnesses.
You may search for a member on the College’s Public Register. Please contact the College staff if you have trouble identifying the member.
You can request to withdraw your complaint. The Registrar or the ICRC will review your complaint and request. If your concerns are serious, the Registrar or ICRC may still decide to continue with the investigation.
Préoccupations et plaintes – les enquêtes
Toutes les plaintes déposées contre les membres de l’Ordre sont étudiées par le comité des demandes de renseignements, des plaintes et des rapports, mais elles ne font pas toutes l’objet d’une enquête. Si un sous-comité de ce comité considère qu’une plainte est frivole, vexatoire, faite de mauvaise foi, sans objet ou qu’elle constitue un usage abusif de la procédure, le sous-comité remet au plaignant et au membre de l’Ordre un avis de son intention de prendre aucune mesure à l’égard de la plainte, et il les invite à soumettre des observations. Après avoir étudié toutes les observations qui lui ont été soumises, le sous-comité décide de faire enquête sur les allégations ou de ne prendre aucune autre mesure.
Your complaint will be assigned to a Case Manager, who will manage the complaint file. The Case Manager will be your contact person at the College and is available to answer your questions.
The College will send your complaint to the member. The member will have a chance to review the complaint and respond. In most cases, the College will request that the member provide the clinical record. At the same time, the College will acknowledge your complaint in writing.
The Case Manager will also conduct further investigation. This can include interviewing witnesses and getting other documents.
When the investigation is complete, the complaint file will go to a panel of the ICRC.
Let the case manager know which information you want to access. The College may be able to get that information by way of summons.
À l’heure actuelle, il faut environ 180 jours (six mois) pour traiter une plainte, depuis le moment où l’Ordre la reçoit jusqu’au moment où une décision est rendue au membre de l’Ordre et au plaignant. La loi permet également à l’Ordre de prolonger ce délai, en avisant le plaignant et le membre.
Toutes les décisions concernant les plaintes sont prises par un sous-comité du comité des demandes de renseignements, des plaintes et des rapports. Chaque sous-comité est formé de deux membres de la profession bénévoles et d’un membre du public nommé au conseil de l’Ordre le lieutenant-gouverneur en conseil. Certaines décisions sont rendues par le comité de discipline et le comité d’aptitude professionnelle, qui sont formés de membres de la profession et de membres du public, conformément au Code des professions de la santé, à l’Annexe 2 de la Loi de 1991 sur les professions de la santé réglementées.
The ICRC is a screening committee. It cannot make findings of fact or credibility. The role of the ICRC is to decide how to best protect the public from possible harm.
For every complaint, the ICRC considers the possible risks of the member’s conduct to the public. The ICRC considers both impact and recurrence risks. If the risks are low, the ICRC may decide not to take any action. If the risks are moderate or high, the ICRC is likely to take some kind of action.
The ICRC has developed a table to help with its consideration of risks. This table is available here.
The ICRC meets in person every month from September to May. The ICRC attempts to meet twice over the summer months.
The ICRC also meets by teleconference throughout the year.
The College will send you a formal acknowledgment of your complaint within 14 days of receiving your complaint.
The Case Manager assigned to your complaint will be in touch with you directly if they need additional information.
If the College is unable to meet the 150-day timeline, the College will let you know. The College will then set new timelines.
The College will send you a copy of the ICRC’s decision once it is finalized.
A panel of the ICRC might not come to a final decision when they consider a complaint. The panel may have some questions for one of the parties or may want more information. They will then need to meet again to reach a decision.
The panel also needs some time to write the decision. College staff is not able to communicate any information about an unfinished decision.
No. The ICRC does not meet with either the complainant or the member. The ICRC reviews information contained in paper or electronic records.
Préoccupations et plaintes – les décisions de l'ICRC
No. Only the Discipline Committee can make a finding of professional misconduct after a hearing.
The ICRC can decide whether to refer allegations to the Discipline Committee. If it does not make a referral, the ICRC can still express concern about conduct and take some action.
The action the ICRC takes will depend on the risks associated with the member’s conduct. Please see more information about the ICRC Risk Assessment Framework.
The ICRC may take a range of actions after an investigation:
-
No further action: A panel may take no further action if it believes there is no risk to the public.
-
Advice: A panel may give advice if it identifies low risks. Advice is meant to help the member avoid future risks.
-
Undertakings: A panel may ask for an undertaking from the member if it identifies moderate risks. An undertaking is remedial and is agreed to by the member. An undertaking can range from a minor change in practice to limitations on the member’s certificate of registration.
-
Caution: A panel may caution a member if it identifies moderate risks. The member must come to the College to receive the caution in person. Cautions are remedial and may include a discussion between the panel and the member. Cautions are not open to the public.
-
Specified Continuing Education or Remediation Program (SCERP): A panel can order a SCERP if it identifies moderate risks. A SCERP is remedial and can include a specific course of study.
-
Referral to the Discipline Committee: If the ICRC identifies high risks, it will refer the matter to the Discipline Committee for a full hearing.
- Referral to a Health Inquiry or Fitness to Practice Committee: Sometimes the ICRC identifies health issues that could affect the member’s ability to practice. In these cases, the panel will refer the matter to a Health Inquiry panel of the ICRC. A Health Inquiry panel can order treatment and monitoring. If treatment and monitoring are not enough to ensure safe practice, the ICRC may refer the matter to the Fitness to Practice Committee.
In the last 5 years (January 2015 to March 2020), ICRC outcomes in relation to 416 cases were as follows:
| Outcome | Number* | Percentage* |
| Withdrawal/closed | 10 | 2% |
| Take No Further Action – F&V † | 55 | 13% |
| Take No Further Action | 157 | 38% |
| Advice | 85 | 20% |
| Written Caution ‡ | 37 | 9% |
| Caution | 17 | 4% |
| Undertakings | 41 | 10% |
| SCERP | 17 | 4% |
| Refer to Discipline Committee | 18 | 4% |
| Total | 437 | 105% |
*The Percentages add up to more than 100% due to multiple outcomes in some cases, i.e. caution and undertaking. The 437 outcomes here relate to 41 cases.
† Frivolous, vexations, made in bad faith, moot, or an abuse of process. See the FAQs above.
‡ As of September 8, 2017, the ICRC no longer issues written cautions.
Les renseignements sur les plaintes sont accessibles au public seulement si les allégations formulées contre un membre de l’Ordre ont été renvoyées au comité de discipline par le comité des demandes de renseignements, des plaintes et des rapports, et seulement si le comité de discipline conclut qu’il y a eu faute professionnelle ou incompétence. Ces renseignements sont publiés sur le site Web de l’Ordre et sont accessibles en utilisant la fonction « Recherche sur les membres ». Les renseignements sur les plaintes précédentes, autres que les plaintes considérées comme frivoles, vexatoires, faites de mauvaise foi, sans objet ou constituant un usage abusif de la procédure, sont mis à la disposition du comité des demandes de renseignements, des plaintes et des rapports lorsque celui-ci étudie une plainte subséquente portée contre un membre de l’Ordre.
Tout membre de l’Ordre et tout plaignant peut demander que la décision soit examinée par la Commission d’appel et de révision des professions de la santé, un organisme indépendant qui rend compte de ses activités au ministère de la Santé et des Soins de longue durée, sauf si la décision rendue consiste à renvoyer l’affaire au comité de discipline ou au comité d’aptitude professionnelle. Après avoir fait l’examen de la décision, la Commission peut prendre une ou plusieurs des mesures suivantes :
-
Confirmer l’ensemble ou une partie de la décision.
-
Recommander au comité des demandes de renseignements, des plaintes et des rapports de prendre les mesures qu’elle considère appropriées.
-
Enjoindre au comité des demandes de renseignements, des plaintes et des rapports de prendre toute mesure que le comité ou un sous-comité est autorisé à prendre vertu de la Loi de 1991 sur les professions de la santé réglementées et du Code des professions de la santé, sauf demander que le registrateur effectue une enquête sur la plainte.
Pour interjeter appel des décisions du comité de discipline, il faut faire une demande d’appel auprès de la Cour divisionnaire de l’Ontario.
No. Section 36(3) of the Regulated Health Professions Act, 1991 does not allow information from a College proceeding to be used in civil court.
Préoccupations et plaintes – rapport obligatoire
You must file a mandatory report no later than 30 days after the reporting obligation has been triggered.
You must file a mandatory report immediately if you believe that:
- The member will continue to sexually abuse a patient or will sexually abuse other patients; or
- That the member is likely to expose a patient to harm or injury.
A report must be filed in writing. Please use the College’s mandatory report form available on the College’s website. You may also write to the College directly through fax, mail or email.
The mandatory reporting form will prompt you for the information necessary with respect to each report. If you have any additional questions about your report, please contact the College at 416-961-8817/1-800-489-8388; or invhear@cpo.on.ca
It may be that your mandatory obligation to report sexual abuse arises in the course of providing psychotherapy to another regulated health professional. In this case, your report must also contain your opinion, if you are able to form one, as to whether this member is likely to sexually abuse patients in the future.
The Inquiries, Complaints, and Reports Committee (ICRC) decides what to do in each case by thinking about the possible negative outcomes of the member’s conduct. The ICRC thinks about this in terms of “risk.”
The ICRC considers both impact and recurrence risks. Impact risks include those to specific individuals, the general public, and the profession. Recurrence risks include concerns about the member’s conduct history, the practices, processes, or systems the member has in place, and the member’s awareness of the practice concerns identified.
The ICRC uses the ICRC Risk Assessment Framework, below, to help categorize these risks. The Framework also helps the ICRC identify the range of appropriate outcomes in relation to the risks.
The outcomes available to the ICRC after the investigation of a complaint or report include:
- No further action: A panel may decide to take no further action if it decides that the member’s conduct poses no risk to the public.
- Advice: A panel may give advice if it identifies low risks. Advice is meant to help the member avoid future risks.
- Undertaking: A panel may ask for an undertaking from the member if it identifies moderate risks. An undertaking is remedial and can range from a minor change in practice to having a mentor.
- Caution: A panel may caution a member if it identifies moderate risks. The member must come to the College to receive the caution in person. Cautions are remedial and may include a discussion between the panel and the member. Cautions are not open to the public.
- Specified Continuing Education or Remediation Program (SCERP): A panel can order a SCERP if it identifies moderate risks. A SCERP is remedial and can include a specific course of study.
- Referral to the Discipline Committee: If the ICRC identifies high risks, it may refer the matter to the Discipline Committee for a full hearing.
Formation continue – exigences du programme
Unless you hold a Certificate of Registration with “Retired” status, you are expected to maintain professional competence, in anticipation of your return to practice. There is a great deal of flexibility in terms of how you may earn CPD credits. While many of the opportunities to earn Category A (Professional Activities) credits involve active professional practice, there are opportunities for credit to be earned that are not directly related to professional practice.
Please note that it is possible to satisfy the requirements of the program by earning as few as 10 credits over two years from Category A. Category B (Continuing Education) credits can be earned outside of the context of active service delivery. If you are experiencing circumstances that make it impossible to satisfy the requirements of the program, please contact the College to discuss this.
Formation continue - administration du programme
While it is expected that you will be continuously engaged in professional development activities, you are only required to declare that you have completed the requirements of the mandatory CPD program at the end of each two-year CPD cycle. Bearing this in mind, you must begin to record credits you earn at the beginning of each cycle. Ordinarily, the cycle will begin on July 1 and end on June 30th, two years later.
Please note: only for members beginning the first cycle in 2017, credits may be collected for the period between May 8th, 2017, and June 30, 2019.
Members with a Certificate authorizing Autonomous Practice or an Inactive Certificate must complete the Self-Assessment Guide (SAG) every two years. Those with a Certificate Authorizing Supervised Practice or Interim Autonomous Practice must complete the SAG every year, however, the CPD cycle is still two years in length, so the CPD declaration must be made every second year. If your current registration number ends in an even number you must begin and end your CPD cycle in years ending in an even number. If your current registration number ends in an odd number you must do so in years ending in an odd number.
The following table indicates when to begin formally recording CPD credits and when your first CPD Declaration of Completion will be due.
| Certificate class and Registration Number at the time a Declaration is required: | Credits earned beginning on the following dates may be counted towards completion of the requirements: | First CPD Declaration Required |
| Supervised Practice « odd » | July 1, 2017* | June 30, 2019 |
| Interim Autonomous Practice « odd » | July 1, 2017* | June 30, 2019 |
| Autonomous Practice « odd » | July 1, 2017* | June 30, 2019 |
| Academic « odd » | July 1, 2017* | June 30, 2019 |
| Inactive « odd » | July 1, 2017* | June 30, 2019 |
| Supervised Practice « even » | July 1, 2018 | June 30, 2020 |
| Interim Autonomous Practice « even » | July 1, 2018 | June 30, 2020 |
| Autonomous Practice « even » | July 1, 2018 | June 30, 2020 |
| Academic « even » | July 1, 2018 | June 30, 2020 |
| Inactive « even » | July 1, 2018 | June 30, 2020 |
*Credits earned from May 2017 will be accepted for this transitional cycle only.
If you have been acquiring CPD credits for two years, regardless of changes to your Certificate of Registration, those credits would apply. In other words, despite any changes in your Certificate of Registration, you will have completed the requirements of the program if you earn 50 credits in the two years leading up to the declaration date. If you receive notice that a declaration is due but have not had a full two years in which to earn the 50 credits, the College will provide you with an alternate declaration that recognizes this.
The Quality Assurance Committee will conduct random audits of member participation in the CPD Program. When audited, members will be required to provide the Quality Assurance Committee with a detailed list of their CPD activities, as well as supporting documentation of their activities, wherever these are available. It is recognized that formal documentation of participation is not available for some activities such as case conferences, self-learning or group viewing of webinars in which individual registration is not required. In such circumstances, formal documentation is not available and members will not be expected to provide it.
Yes. If you are selected for a Peer Assisted Review, the reviewer will request access to your record and documentation of your CPD activities.
Formation continue – activités éligibles au crédit
The intention of the program is to ensure that within a two year period, members are engaged in at least the minimum amount of required professional development. For that reason, only activity within the two years prior to a declaration of completion may be counted.
The categories are comprehensive and it is expected that every CPD activity can be included within one of the categories provided in the program description and tracking sheet available from the College. Examples provided of the activities within each of the categories convey the range of activities members may count. It should be noted that these lists are examples and are not intended to be all-inclusive. Members are expected to use their own judgment in deciding whether the particular activities they choose meet their professional development needs, as identified in the Self-Assessment Guide, and which particular requirements of the CPD program each activity will satisfy.
A peer can be a professional in the field of psychology or a person who is qualified as a professional in a field relevant to the practice of psychology. Interdisciplinary interaction is encouraged by the College.
Professionally relevant programs/workshops are those events that enhance knowledge relevant to the psychological services a member provides. Content need not be primarily psychological in nature but must be directly related to the services provided by the member. For example, a member working within the correctional system might benefit from an educational event provided by correctional officers regarding the management of offenders within the prison system.
If you have earned “CE” credits by attending live events like conferences and conventions you may claim credit for attendance at the conference or convention under Category A and also for the specific time you spend within the presentations as CE credits in Category B. For example, if attending a convention from 9 a.m. until 4 p.m., you would earn one credit for spending the day with peers under Category A8 and, if attending presentations for 4 hours, an additional 4 credits under Category B for the 4 hours you were engaged in learning during the presentations
The College doesn’t accredit or approve courses. Members must determine whether an activity is suitable for CPD credit. If the activity is relevant to one’s CPD, it is eligible for credit. Similarly, the College also doesn’t approve or endorse specific CE accreditation bodies. Members are expected to use their own judgment in determining the appropriateness of specific CE crediting organizations.
Any activities relevant to your Ontario practice are eligible for credit, wherever they take place.
Yes.
Examples of how to satisfy this requirement include participating in any professional activity or continuing education activity related to ethical issues, including those addressing local jurisdictional issues. The following are a few examples of the many ways you may earn these credits:
-
Attending an event run by a local professional group or participating in an organized discussion group that addresses professional ethics
-
Working with a workplace ethics committee
-
Attending the Barbara Wand Symposiums, in person or by webinar, or watching the archived recordings
-
Completing online continuing educational programs offered by professional associations
-
Participating in a College or professional association activity related to ethical practice
-
Attending, or watching webcasts of public lectures which are offered by universities and other educational organizations that are relevant to professional ethics
-
Reading books and articles that are relevant to professional ethics
Teaching psychology requires ongoing research, up-to-date knowledge, and an ongoing exchange of information between teachers and students. For this reason, it is regarded as valuable CPD.
Formally monitoring progress towards specific outcome goals, either for individual clients or on an organizational level, can be a useful mechanism for determining whether an approach to practice is effective or not and is a valuable learning experience. Active participation in either activity is eligible for CPD credit.
It is recognized that Conducting Formal Research is a distinct activity and that not all of those involved in conducting research are responsible for writing about it. Additional credit may be obtained for writing, reviewing, and editing in Category A4.
The CPD program is intended to ensure that you maintain competence within your existing authorized areas of practice and with your authorized client populations. The development of competence in additional areas of practice or with additional populations must be undertaken through a much more comprehensive and rigorous process, beyond what would ordinarily be required to satisfy the CPD requirements. If you are seeking to expand your areas of authorized practice or authorized client populations, please contact the College.
If participating in your own therapy leads you to gain knowledge, experience, and/or skills that advance your ability to provide professional psychological services it may be counted as one type of activity under category A1 for a maximum of ten credits every two years.
Peer Review under category A1 (Professional Consultation/ Interaction) is meant to include peer review of another member’s practice. Reviewing another member’s professional reports could be counted under category A1 as it is a form of professional consultation. Reviewing articles for publication may be counted under category A4 (Writing, Reviewing, Editing).
Formation continue – Catégorisation des activités
The College will require you to provide a declaration that you have satisfied all of the requirements of the program at the end of each two-year CPD cycle. You will not be required to provide details describing your CPD activities, or supporting documentation unless the College specifically asks you to do so.
This may occur when:
- You have not submitted your Declaration of Completion of the CPD requirements by the College’s deadline
- You have been selected when the Quality Assurance Committee conducts a random audit of member participation in the CPD program
- You are subject to an Assessment or Review under the College’s Quality Assurance Program, including a Peer and Practice Assessment
Category A (Professional Activities) includes activity-based experiences believed to enhance professional development by developing competencies in the multifaceted areas related to one’s practice. In addition to keeping abreast of scientific knowledge, members are encouraged to include other components of service enhancement in their CPD activities. Examples of these include but are not limited to, reviewing evidence for the purpose of evidence-based decision making, keeping up to date with technology, and enhancing interpersonal and multicultural competence.
A maximum of 10 credits for any one type of activity may be counted in section A1. If what you do in the peer consultation group is different than what you would do in the individual consultations, then you could consider it to be two different activities and you could acquire 20 credits in all. There will be judgment calls to be made when deciding ‘what belongs where’ and we are leaving it up to members’ own good judgment to make these decisions, so long as they can provide a reasonable rationale for the decision if asked for one. Incidentally, you can earn peer consultation credits for consulting with any professionals, not only psychologists and psychological associates, if the discussion is with a professional and the issues are relevant to your practice.
Credit for general attendance at events in Category A8 is meant to reflect the value, in and of itself, inherent in interacting with colleagues and participating in the social, interpersonal, professional, and scientific activities which are part of the milieu of conferences and conventions. It is believed that being among peers enhances professional development as this leads to awareness of the practices of colleagues and of the ideas, problems, and challenges that are present in the professional environment. Continuing Education credits available under Category B reflect the acquisition of information from attending presentations while at the event. This applies whether the events are attended in person or via technology.
No, the 10 credits related to ethics are not additional credits. You must ensure that a minimum of 10 of the credits earned in satisfaction of the 50 credits required in total are related to professional ethics.
Formation continue – Documenter les activités
Many conferences and workshops provide participants with a certificate of attendance and this would be sufficient verification. For organized events that do not provide such certification, a record of your registration or payment will suffice. For other activities where formal documentation is not provided, like case rounds, self-guided learning, time spent conducting research or observing a webinar with a group where individual sign-up is not required, you may simply state that you have participated in the activity and provide a description of the activity including the organization, group, people, publication and/or other resources involved. Here is a sample completed CPD tracking form which provides the level of detail suggested.
The College will not require you to pay for an “official CE credit” document. Your statement, program information from the provider indicating that formal CE credits are available and confirmation of registration will be sufficient.
No. The electronic tracking tool has been developed as an aid for members who wish to use it. So long as you maintain an accessible record of your CPD activities, you may keep track of them in any manner you wish.
You must retain your records for at least five years after completion of your last CPD cycle.
Évaluation Par Les Pairs
The Peer Assisted Review (PAR) process has been in place since the fall of 1999. Each year, a number of members are randomly selected to have their practices reviewed as part of the College’s Quality Assurance Program. The PAR is described below in a series of FAQ’s, in an effort to provide members with an understanding of the process.
Any member with a Certificate of Registration for Autonomous Practice is a potential participant in the PAR process.
Any member who has not completed the mandatory Self-Assessment requirement of the College is required to participate in a PAR. Additionally, members are identified for participation using a computerized random, or stratified random, selection process.
Two members of the College; an assessor appointed by the Committee and a reviewer nominated by the member being reviewed.
Generally, both the assessor and the reviewer will have knowledge of the member’s area(s) of practice, population(s) served and practice setting(s).
The member undergoing a review will have an opportunity to indicate whether they believe that there is any reason a potential assessor should not conduct the review.
Efforts are also made to select an assessor who has either undergone a review themselves or who has previously acted as an assessor or reviewer.
The reviewer is nominated by the member being reviewed and can be a colleague or associate. They may act as a support to the member. While this individual is nominated by the member being reviewed, in accepting this role the reviewer understands and agrees to act as an agent of the College and therefore to act in the public interest.
The assessor and reviewer must undertake and agree to:
- Participate in the College’s Peer Assisted Review Assessor and Reviewer training before conducting the review, if I have not already done so within one year prior to the date of the review
- Maintain confidentiality, as required by s.36 of the Regulated Health Professions Act, 1991, S.O. 1991, c. 18
- Familiarize themselves with the Legislation, Regulations and the Standards of Professional Conduct relevant to the practice they will be reviewingand attest that:
- They have held a certificate of Registration for Autonomous Practice with the College of Psychologists of Ontario for at least five years
- They are currently in active practice as a psychologist or psychological associate
- They are free of any conflict of interest or bias, or any appearance of either, with respect to the review
- Neither themselves, nor the individual they will be reviewing is in a position of power with respect to the other
The review is conducted at the member’s practice setting. In cases where a member works in more than one setting, the appropriate location for the review will be determined in discussion with the member.
Members normally set aside a morning or afternoon for the review as it can take from three to four hours.
The scheduling is determined by the assessor and reviewer, in consultation with the member being reviewed. It is expected that every effort will be made to schedule the review at a mutually agreeable, and convenient time for all participants and which takes into account the least disruption to the member’s work schedule.
The assessor and reviewer will together observe the member’s place of practice, interview the member using a structured interview form and review some of the member’s clinical records.
The Reviewers will provide a report to the Quality Assurance Committee. The Committee appointed assessor must provide a copy of the report as well as notice of the right to make submissions to the Quality Assurance Committee within 14 days of receipt of the report, directly to the individual who has been reviewed.
The Quality Assurance Committee will review the Report and any submissions the member has made and determine whether any action is required, in the public interest.
One of three outcomes is possible from the review:
- Meets Standards without any qualification: This is a relatively frequent outcome in which no areas for improvement are identified. Some suggestions may be offered by the reviewers that the member may find helpful to incorporate into his/her practice.
- Would meet Standards with minor modifications: This is a relatively frequent occurrence in which minor areas for improvement are identified which the member has agreed, with the reviewers, to address within a specified time frame. The Quality Assurance Committee will confirm with the member and the reviewers that the recommended and agreed upon changes have been completed.
- Is Significantly Below Acceptable Standards: While this is not a frequent occurrence, when major areas for improvement are identified, the Quality Assurance Committee will address these directly with the member.
If you have any questions regarding the PAR please don’t hesitate to contact Madeleine Lee,
Quality Assurance Coordinator at qualityassurance@cpo.on.ca
Sociétés professionnelles
The word “ancillary” is not defined in the Business Corporations Act, 1990 from which this condition arises. It’s the College’s position that, in this context, it means subordinate, subsidiary, or secondary to the practice of psychology. Despite similarities in the practices, Social Workers, Social Service Workers and Registered Psychotherapists are practicing distinct other professions.
Psychology may only be practiced in Ontario by members of the College of Psychologists or those supervised by them. Professional services provided by autonomous practitioners of different professions would not be considered the practice of psychology. It’s the College’s understanding that the practice of other professions would not be considered to be ancillary to the practice of psychology.
While both are corporations, the rules that stipulate their ownership structures and the activities that they can undertake are different.
Professional Corporations
The shareholders of professional corporations must all be members of the same health regulatory college as must all the officers and directors of the professional corporation. Further, the only business that a professional corporation is permitted to undertake is the practice of the profession and activities that are related to or ancillary to the practice of the profession. Every professional corporation is also required to obtain a Certificate of Authorization from the college of its members before it is permitted to conduct its business.
Practice Management Corporations
In contrast, the ownership rules of corporations that manage practices are more relaxed. Members of different health professions, non-health professionals and even family members can be shareholders as well as officers or directors. Corporations that manage practices are not permitted to practice any regulated health profession and the shareholders of these corporations are not permitted to practice their regulated health profession through the corporation. This does not mean that members cannot work for non-professional corporations owned by others. Rather, it means that when they are working for a such a corporation, they are practicing as individual health professionals outside of the corporation. Because these corporations are not permitted to practice a regulated health profession, they are not required to register with the College or Colleges of their shareholders.
The College is not in a position to legal advice with respect to the Business Corporations Act. Your legal and business advisors can provide specific advice relevant to your circumstance.
There are differences between professional corporations and those that manage practices and are not professional corporations. A corporation that manages a practice, and is not a health professional corporation, is not permitted to practice a regulated health profession and hence is not required to register with the College or Colleges of their shareholders.
The College is not in a position to legal advice with respect to the Business Corporations Act. Your legal and business advisors can provide specific advice relevant to your circumstance.
This is a business decision. The College recommends that you discuss your plans with an accountant or lawyer who specializes in this area.
No, if you are practising the profession of psychology through a corporation it may only be a psychology professional corporation that operates under a Certificate of Authorization issued by the College of Psychologists of Ontario.
Members who wish to practise through a corporation are required to obtain a Certificate of Authorization from the College. Detailed information and application forms can be found on the College Website.
You may submit the application and supporting documents via email to corporations@cpo.on.ca
Or by regular mail* to:
110 Eglinton Avenue West
Suite 500
Toronto, Ontario M4R 1A3
You may submit the application fee in the following ways:
- Electronic Bill Payment may be made through web banking.
- Email Transfer payments may be sent to payments@cpo.on.ca. Please use CPO + your registration number as the password (ex. CPO####)
- Mail* a Cheque to the College.
*Please send only via regular mail as we are unable to accept courier packages at this time.
Once a complete application package has been received by the College, it takes 2 to 3 weeks for processing. The effective date of the certificate is the date the complete package and application fee was received.
The application fee for a new Certificate of Authorization is $350.
There are restrictions on the names of professional corporations. Please refer to the College Guide to an Application for Certificate of Authorization for Professional Corporation. Briefly, the names of professional corporations must:
- Include the surname of one or more shareholders of the corporation as the surname is set out in the College register;
- Indicate the health profession practised by the shareholders (i.e. “psychology”);
- Include the words “Professional Corporation” or “Société professionnelle”.
For detailed information, please refer to section 3.2 of the Business Corporation Act, 1990 and Ontario Regulation 39/02 under the Regulated Health Professions Act, 1991. It is also wise to consult with the College before setting up your corporation to ensure that the name is appropriate.
Examples: Smith Psychology Professional Corporation; Smith and Jones Psychology Professional Corporation; John Smith Psychology Professional Corporation; J. Smith Psychology Professional Corporation.
You may use a different practice name than the name of your professional corporation. You must list every practice name under which the professional corporation practices when completing the application form.
Speak to your own lawyer or accountant about the requirements for registering business names.
The College does not approve or comment on practice names, and there are no specific rules for practice names other than to ensure the name does not violate the section of the Advertising Regulation, (see section 18.1) This section prohibits in advertising, and so also in naming, something that would suggest uniqueness, specialty or something that is false or misleading.
Only members of the College of Psychologists of Ontario.
Yes, if all the shareholders, officers and directors of the holding company are registered members with the College of Psychologists of Ontario.
No. Members intending to incorporate must do so under the Ontario Business Corporations Act. For forms and instructions on how to incorporate, contact the Companies Branch of the Ministry of Government Services website or call 416-314-8880.
Health profession corporations incorporated in a jurisdiction outside Ontario, including corporations federally incorporated under the Canada Business Corporations Act, cannot obtain a Certificate of Authorization from the College. They must incorporate under the Ontario Business Corporations Act, and satisfy the conditions and requirements of the RHPA to be considered a health profession corporation in Ontario.
The certificate is valid for one year and must be renewed annually on the date of authorization. Members will be emailed a renewal package approximately 6 weeks prior to this date.
The fee for renewal of a Certificate of Authorization is $250.
The requirements related to issuance and renewals of Certificates of Authorization are set out in the Regulated Health Professions Act, 1991 (RHPA) and the Certificates of Authorization Regulation. They apply equally to all regulated health professions in Ontario. The general requirement for annual renewal is written into these regulations as a fixed component. The College asks members to complete only what is required under the RHPA.
A Corporation Profile Report is a document issued by the Ontario Ministry of Government and Consumer Services that indicates that the corporation is registered and active. The legislation sets out the requirements for the annual renewal of your Certificate of Authorization. One of those requirements is that a current-dated Corporation Profile Report accompanies your annual renewal application regardless of how long your health professional corporation has been in existence.
You may obtain a newly issued Corporation Profile Report by:
- Contact the Ministry of Public and Business Service Delivery (formerly the Ministry of Government and Consumer Services) directly:
- 375 University Avenue, 2nd Floor, Toronto, M5G 2M2 | Tel: 416-314-8880 or 1-800-361-3223
- https://www.ontario.ca/page/ontario-business-registry
- Using any online websites that provide the service to generate the report
The Corporation Profile Report does not need to be certified.
You must submit articles of amendment filed with the Ministry of Government Services if you made any changes, such as a name change, to the corporation since incorporation or the last renewal.
Yes – In fact, the College must revoke a professional corporation’s Certificate of Authorization in a number of circumstances. These include:
- The corporation ceases to be eligible to hold a Certificate of Authorization.
- The corporation ceases to practise the profession in respect of which the Certificate of Authorization was issued.
- The corporation fails to comply with one or more of the requirements for a renewal of the Certificate of Authorization.
- The corporation carries on any business that is not the practice of the profession governed by the College or activities related to or ancillary to the practice of that profession.
If the College revoked a Certificate of Authorization, the professional corporation must apply for a new one and meet the eligibility requirements in effect at the time of the new application. At that time one must submit the required application and supporting documents and pay the application fee.
Professional Practice
Originally published in Volume 2 Issue 1 of HeadLines.
The answer to this question depends upon various decisions made by the organization, including who is the Health Information Custodian (HIC), a term which is used and defined in the Personal Health Information Protection Act, 2004 . For the purposes of answering this question, either a health care practitioner or a person who operates a group practice of health care practitioners may be a HIC. There may only be one HIC and it should be the person who will have ultimate responsibility for the collection, use, disclosure, security, and retention of the information. .
The HIC must ensure that their identity is made clear to all concerned, including the client. A client must provide informed consent for a specified individual or organization to collect information about them.
A Health Information Custodian may have an “agent”. This is defined in PHIPA as a person that, with the authorization of the custodian, acts for or on behalf of the custodian. The HIC may, for example, appoint the service provider working in the HIC’s organization to be their agent.
Copies of information may be shared with those with a need to have the information in their possession but may only be provided to anyone other than the HIC or agent with client consent. The number of copies of the same information is directly correlated to the risk of loss or unauthorized access to the information. The fewer number of copies there are of a document, the lower the risk of loss or unauthorized disclosure.
There is no prohibition against storing information in more than one file/location. Standard 9.1 of the Standards of Professional Conduct, 2017 requires that a member must make best efforts to ensure that the member’s records are complete and accessible; this applies whether the record is kept in a single file or in several files and whether the record is housed in one location or at several locations. It is suggested that when records are not maintained in one file or location that a note is placed in each location indicating the location(s) of any other information.
Originally published in Volume 2 Issue 1 of HeadLines.
In the practices of most members, the answer to this question can be found in the Health Care Consent Act, 1996 (HCCA) and the Personal Health Information Privacy Act, 2004 (PHIPA).
One must first establish whether the child has the capacity to make their own independent decisions in these situations. The HCCA and the PHIPA do not specify chronological ages of consent but instead set out the test for determining whether any individual, including a child, is capable of making their own health care decisions. The determination of capacity must be made by the Health Care Provider or the Health Information Custodian, as the case may be. The analogous tests for capacity to be applied are set out in section 4 of the HCCA and section 21 of PHIPA, respectively.
If the child is not believed to be capable, a substitute decision-maker for the purpose of the HCCA is generally deemed to play the same role with respect to PHIPA.
Section 20 of the HCCA and Section 26 of PHIPA provide specific advice with respect to the hierarchy of potential decision-makers when a child is not believed to be capable of making their own decisions. It also sets out the mechanisms for deciding what must happen when a person with the right to make decisions is not available or willing to assume decision-making responsibility. The legislation also addresses what to do if there is conflict between two individuals having equal ranking in the hierarchy.
Generally, a parent can give or refuse consent on behalf of an incapable child unless this authority has been lawfully granted to a children’s aid society or other person. If both parents do not have the same rights under an Agreement or Order, a parent with custodial rights prevails over a parent who has only a right of access. In situations where the statute does not spell out clearly which parent is entitled to make the decision, statutory interpretation is necessary. Given the high stakes for all individuals involved, the most prudent course of action is to obtain independent legal advice.
The College’s August 2005 Bulletin provides additional guidance with respect to this issue.
The provision of psychological services is regulated locally within most North American provinces, states and territories, for the purpose of protecting those located within the province, state, or territory.
In most jurisdictions, including Ontario, services are deemed to be delivered in the location of the client. Each jurisdiction has its own statutes and regulations and has the authority to take action with respect to unauthorized practice. For this reason, permission must be sought from the College or Board in the same province, state or territory as the person who will be receiving services is physically located.
The College of Psychologists of Ontario does not have the authority to grant permission to provide psychological services anywhere other than in Ontario. College members may provide services in other jurisdictions wherever they are permitted to by the psychology regulatory body in that jurisdiction, so long as they do so in accordance with the Standards of Professional Conduct, 2017.
Ontario statute requires that one must be a member of the College of Psychologists of Ontario, or supervised by a member of the College, to provide psychological services to a person located in Ontario.
The Psychology Act, 1991 states:
Restricted titles
8 (1) No person other than a member shall use the title “psychologist” or “psychological associate”, a variation or abbreviation or an equivalent in another language.
Representations of qualification, etc.
(2) No person other than a member shall hold himself or herself out as a person who is qualified to practise in Ontario as a psychologist or psychological associate or in a specialty of psychology.
Idem
(3) A person who is not a member contravenes subsection (2) if he or she uses the word “psychology” or “psychological”, an abbreviation or an equivalent in another language in any title or designation or in any description of services offered or provided.
Exception for university faculty
(4) Subsections (1) and (3) do not apply to a person in the course of his or her employment by a university.
Temporary, limited membership is available to individuals licensed to provide psychological services in other jurisdictions allowing them to provide services for a period of up to 12 months, if:
- The client is located temporarily in Ontario for a period of up to 12 months
- It would be clinically ill advised or impractical to transfer psychological services to a practitioner already registered with the College
- The practitioner is eligible to work in Canada and be registered/licensed with a psychology regulatory body which:
- is in one of the Canadian provinces or territories;
- has entered into a written reciprocity agreement with the College;
- has requirements substantially equivalent to those of the College for a certificate of registration for a psychologist or psychological associate authorizing autonomous practice; or
- holds a current certificate of Professional Qualification (CPQ) awarded by the Association of State and Provincial Psychology Boards (ASPPB).
To learn more and to apply for this form of membership please click here.
In order to provide psychological services to an individual located in Ontario, or hold out as qualified to do so, the Psychology Act, 1991 requires that one must be a member of the College of Psychologists of Ontario, or be working under the supervision of a member of the College. There may be circumstances in which there is a need to include, by way of videoconferencing or teleconferencing, an individual located in Ontario in a session conducted with your clients in your own home jurisdiction. So long as the involvement of the person in Ontario is limited to their role as a resource in treating or assessing the clients in your own local jurisdiction, and not for the purpose of treating or assessing the individuals located in Ontario, they may be included. In such a case, they may be considered a collateral resource for the benefit of the clients receiving your service in your own jurisdiction.
The Psychology Act, 1991 limits the provision of psychological services in Ontario to members of the College of Psychologists of Ontario. In the absence of legislative amendments, the College is not able to authorize anyone other than members of the College to provide telepsychology services to clients located in Ontario.
Under normal circumstances, the College views such activities by non-members as « unauthorized practice » and considers whether there is a need for appropriate action. The College has carefully considered the extreme circumstances in which we find ourselves. We recognize this must be taken into account with regard to duly registered/licensed practitioners from other jurisdictions who must provide telepsychology services into Ontario for their existing clients during the current emergency situation.
Therefore, in response to the urgent COVID-19 situation, the College will not initiate an « unauthorized practice » action against an out of province practitioner provided the practitioner is:
- registered/licensed in good standing in another jurisdiction at the time the services are provided;
- practices only within their areas of competence and in accordance with any terms, limits and conditions on their license/certificate of registration; and
- only provides the services to:
– existing clients temporarily in Ontario due to the COVID-19 situation when it is clinically ill-advised to temporarily stop services and/or to transfer the service to a member of the College of Psychologists of Ontario;
– clients who are temporarily located in Ontario due to the COVID-19 situation and are entitled to receive those services as a benefit of their registration with a University or College or other benefit program outside of Ontario, where the services will be provided by an out of province practitioner on behalf of the University or College counselling service or other benefit program; or
– clients who are temporarily located in Ontario due to the COVID-19 situation, when it is reasonably expected that the clients will require continuing services with the same practitioner upon the client’s return to the jurisdiction in which the clinician is registered.
Out of province practitioners are asked to confirm their understanding and acceptance of the requirements listed above by notifying the College of their intention to provide telepsychology service to existing clients in Ontario. Practitioners should email the College (cpo@cpo.on.ca) providing their name, the jurisdiction in which they are registered/licensed, and their registration/license number. While the College will endeavour to acknowledge receipt of this information, practitioners need not wait for confirmation before initiating service.
The Standards of Professional Conduct, 2017 state that:
11.1 Fees and Billing Arrangements
Members must reach an agreement with an individual, group or organization concerning the psychological services to be provided, the fees to be charged and the billing arrangements prior to providing psychological services. Any changes in the services to be provided must be agreed to by the client before service is delivered or fees are changed. Fees must be based on amount of time spent and complexity of the services
rendered.
Practical Application: Fees for services should be determined on a consistent basis, regardless of the payer. A member may, however, offer pro bono services or apply a sliding scale to ensure access to services and affordability.
While this Standard is most often thought of in the context of initiating services with a new client, it also can be read to apply with respect to the ongoing provision of services. That is, “providing psychological services” could be read to mean each instance of providing a psychological service. It would be inappropriate for a client to learn that their fees had been increased when they receive a bill for a service that had already occurred. Increased fees may be an important consideration for clients in the ongoing informed consent to service process and some clients may need to reconsider whether they are able, or prepared, to continue at the new proposed rate.
There is no specific period of notice for a fee change set out in any Regulations or in the Standards as this is a matter of professional judgment. Adequate notice of the change however, is important and there may be clients who experience a fee increase as akin to indirect termination of therapy.
In cases where the client may not agree to an increased fee, and a member is not prepared to continue to provide services at the existing rate, guidance regarding the termination of services can be found in section 8 of O.Reg. 80.1/93: Professional Misconduct. This section of the Regulation states that termination of service that is needed is an act of professional misconduct unless:
i. the client requests the discontinuation,
ii. the client withdraws from the service,
iii. reasonable efforts are made to arrange alternative services,
iv. the client is given a reasonable opportunity to arrange alternative services, or
v. continuing to provide the services would place the member at serious personal risk.
Although there are informal ‘rules of thumb’ with respect to ‘winding down of therapy’, often based upon the length of time a person has been receiving treatment, the College does not set any particulars in this regard. If the client requires additional services but can not or will not pay the increased rate, it would be reasonable and appropriate to work with them for a time period that, in the member’s professional judgment, is sufficient to arrange for a transfer of care to another service provider and avoid any harm due to a disruption of treatment.
This can be the case with respect to such factors as age, language, race, culture, or gender diversity and is a legitimate concern. In the absence of appropriate norms, one would need to use clinical judgment to interpret the client’s response to items and, in accordance with the following Standards:
A member must render only those professional opinions that are based on current, reliable, adequate, and appropriate information.
The answer to this question depends upon who has been identified as the Health Information Custodian. Under the Personal Health Information Protection Act, 2004 (PHIPA), it is possible that either a health care practitioner or a person who operates a group practice of health care practitioners can act as the Health Information Custodian (HIC). While either is possible, only one must be established at the onset of services. Generally, this will be the particular individual or entity they authorize to collect their Personal Health Information.
If, in this scenario, the operator of a group practice is not the HIC, then, the following Standard is applicable:
4.1 Responsibility of Supervisors of Psychological Service Providers
If members are supervising psychological services provided by a member holding a certificate for supervised practice or any other unregulated or regulated service provider who is not an autonomous practice member of the College, the clients are considered to be clients of the supervisor…
It then follows that the records are considered to be the records of the supervising member. This is supported by the following additional Standard:
9.1.2 Members Responsible for Supervising Supervised Practice Members and Non- Members
Members supervising Supervised Practice members and non-members are responsible for the security, accessibility, maintenance, and retention of records.
If the organization is not the HIC, at the end of the engagement, in most case it is the supervising member who is the HIC and the records must remain with them for the required retention period.
A member must identify limits to the certainty with which diagnoses, opinions, or predictions can be made about individuals or groups.
An American Psychological Association article about assessing people who are transgender provides one example of how to conduct an assessment where no appropriate norms have been identified. In the absence of specific guidance concerning an identified group, registrants are advised to document their approach to interpreting test responses. This can be helpful in the event that assessment results are challenged and, of at least as much importance, the exercise of writing out a rationale can help make the activity as objective as possible.
In order to answer this question, it is important to consider what is meant by “consulting” as it can be understood to mean different things in different contexts. Consultation is defined in the Standards of Professional Conduct, 2017 as:
the provision of information, within a relationship of professionals of relatively equal status, generally based upon a limited amount of information that offers a point of view that is not binding with respect to the subsequent professional behaviour of the recipient of the information.
If this describes the nature of the relationship with the agency, then the organization is generally considered to be the client. In the case of an organizational client, the member providing consultation is required to maintain records in accordance with the following Standard:
9.3 Organizational Client Records
1. Members must keep a record related to the services provided to each organizational client.
2. The record must include the following:
a) the name and contact information of the organizational client;
b) the name(s) and title(s) of the person(s) who can release confidential information about the
organizational client;
c)the date and nature of each material service provided to the organizational client;
d) a copy of all agreements and correspondence with the organizational client; and
e) a copy of each report that is prepared for the organizational client.
The “nature of each material service provided to the organizational client” in c) above, should likely include sufficient information to address queries about the quality of the particular consultation, should that information ever be needed.
An organizational client record must be retained for at least ten years following the organizational client’s last contact. If the organizational client has been receiving service for more than ten years, information contained in a record that is more than ten years old may be destroyed, if the information is not relevant to services currently being provided.
It is the responsibility of the individual providing services to ensure that proper client consent is obtain for the service being providing. A person acting as a consultant to a service provider would not likely be in a position to seek consent from the person receiving services from the consultee. The consultant may, in fact, never come into contact with the person receiving services from the consultee. In some cases they may not even know their name.
If a member is identified as a “consultant” but they are personally providing the psychological assessment, diagnosis, opinion or intervention, as opposed to “consulting” to or supervising another service provider, this would likely be considered a direct service. In this case, all of the Standards relevant to direct service provision, including those pertaining to consent and record-keeping, would be applicable.
In circumstances where it is unclear whether one is providing direct service or consultation, it may be useful to ask: Is this a service I would provide autonomously to an individual or family in a clinical practice, or is it providing advice to another autonomous service provider who is simply looking for the input with respect to clinical decisions they must make themselves?
Most of the queries we have received related to this problem have been asked in the context of an individual who is transgender, where a client may be capable of making their own decisions may not be in a position to effect a legal name change, due to age or an institutional or family situation. Ideally, such issues should be discussed as part of the informed consent process, as early as possible and preferably before beginning the assessment. If the client agrees to have both their legal and preferred names in the report, that would avoid any confusion to readers of the report with respect to who the report is about. If the client does not provide permission to note both names and there is a need to include the client’s non-preferred name, or to indicate that the name used in the report is not the same as the client’s legal name, this will require careful navigation, in order to protect the client’s dignity and to avoid making a potential misrepresentation. In such a case, it would be prudent to obtain independent legal advice before proceeding.
When addressing issues related to a trans person’s identify, the Ontario Human Rights Commission provides the following guidance:
- Preventing discrimination because gender identity and gender expression – 9 reasonable bona fide requirements
2. Preventing discrimination because gender identity and gender expression – 7 forms of discrimination
3. Preventing discrimination because of gender identity and gender expression – preventing and responding to discrimination
This article, by the APA provides some guidance for how to determine when treating two ‘related’ individuals could become problematic.
In summary, the decision about whether or not to take on individual clients who are related either through family, friendship or are involved with each other in any other way will depend on a critical evaluation of the circumstances, nature of that relationship and the potential for cross involvement at any time.
We recognize that ‘word of mouth’ is often how clients find their therapists, so it is likely that many members have clients who know each other. Each situation will likely present different risks and degrees of risk. When separately treating individuals who are friends with each other, there is a possibility that one client may want to discuss the other client for a variety of possible reasons. This could be problematic if the information they want to share is related to the issues you are treating the other person for and that information may be relevant to your formulation of the other case, regardless of whether or not it is verifiable information. In other words, this could be seen as a problem with respect to protection of both confidentiality and objectivity. Working with clients who you know to be friends with each other should be avoided whenever possible due to the complications that can arise. and increase the possibility that you may contravene the following Standards of Professional Conduct:
8.1 Collection, Use and Disclosure
Members are responsible for ensuring that consent is obtained with respect to the collection, use and disclosure of personal information and personal health information in a manner required by legislation applicable to the relevant service.
10.5 Freedom from Bias
Members must provide professional opinions that are clear, fair and unbiased and must make best efforts to avoid the appearance of bias.
13.1 Compromised Objectivity, Competence or Effectiveness Due to Relational Factors
Members must not undertake or continue to provide psychological services with an individual client when their objectivity, competence or effectiveness is, or could reasonably be expected to be, impaired. This could be due to the members present or previous familial, social, sexual, emotional, financial, supervisory, political, administrative, or legal relationship with the client or a relevant person associated with the client. This prohibition does not apply if the services are delivered to an organizational client and the nature of the professional relationship is neither therapeutic nor vulnerable to exploitation.
This article, published by the American Psychological Association provides an example of the difficulties which could arise when treating two ‘related’ individuals could become problematic.
A decision about whether to take on individual clients who are related either through family, friendship or are involved with each other in any other way will depend on a critical evaluation of the circumstances, nature of that relationship and the potential for cross involvement at any time. While treating individuals who are associated with each other is not strictly prohibited, if the community is large enough, it would be better to find another practitioner who would not be in such a potentially challenging situation.
As you likely know, dual relationships are not strictly prohibited but should be avoided, unless the client is unable to find another competent and available service provider.
Before agreeing to provide the service, you may wish to think about whether your previous professional relationship could lead to any concerns that this assessment was anything less than highly objective. While you are likely to work hard to remain objective, this can be difficult if you do hope for a particular outcome for a client you have supported through their struggles. Even if you can be perfectly objective, if your findings were to be challenged, it could be alleged that you weren’t, due to your previous alliance with the client.
It would also be important to consider whether there is any possibility that the client may seek intervention from you in the future, and whether your role as an assessor might prevent them from doing so. This could be the case if they were unhappy with the outcome of the assessment and this prevented them from returning to therapy with you, causing them to have to “start all over again” with another therapist.
Although multiple relationships are not strictly prohibited, the College has observed that members trying to be helpful by having multiple different service relationships with the same clients have inadvertently entered into challenging situations.
While the College Standards set out the minimum length of time for record retention, there are no rules against keeping information indefinitely. It is not advisable though, to keep information which is not likely to be useful any longer than one needs to, due to the risks associated with unauthorized access to any record.
It’s our understanding that many members do keep a log of the files they have destroyed, with information such as you have outlined in your question. It is important to know that the information in such a record is considered Personal Health Information and that these lists themselves are subject to the same privacy legislation and Standards as the records themselves were, because they identity individuals who have received health care. If you do decide to keep such a record you might also consider including the date of destruction
Following the successful completion of an Oral Examination, and after you are issued a Certificate of Registration authorizing Autonomous Practice, you will no longer require supervision in your authorized areas of practice and client populations. Although formal supervision is no longer required, consultation and other forms of peer support can be of great value throughout your professional career.
Under Supervised Practice, your supervisor was responsible for your adherence to the Legislation, Regulations, Standards and Ethical Guidelines applicable to your practice. If you have been issued a Certificate of Registration authorizing Autonomous Practice you are now fully accountable for the discharge of your own professional and ethical responsibilities.
While the applicability of various statutory and ethical obligations can be straightforward when taking on new clients, taking on the management of professional responsibilities with clients who were initially seen under supervision often leads to questions about such matters as informed consent, fees and billing, and clinical records.
Continuing to Work with Clients you had Previously been Supervised with
If you will be continuing to work with individuals who you worked with during your period of Supervised Practice, it is important consider the changes your new Autonomous Practice registration entails. It’s important to:
- Ensure that clients who wish to continue working with you as an autonomous practitioner, know that you will now be solely responsible now for their care, that your supervisor no longer considers them to be their clients and that you are no longer under supervision;
- Engage in an independent informed consent process with clients, outlining your new, autonomous professional responsibilities and confirm agreement with respect to what services you will be providing, and on the fees you will be charging;
- Clarify that the personal health information collected during your period of Supervised Practice must remain with the person or organization who was the Health Information Custodian during your supervision;
- If you are to be considered the Health Information Custodian going forward, you may obtain a copy of records made to date only with the client’s consent; information about who is the Health Information Custodian can be found here: Who “Owns” the Clinical Record? In a group practice comprised of members authorized for autonomous practice, who can access, contribute to, and hold copies of the clinical record?
A member of the College of Psychologists of Ontario may provide services to clients located in Ontario, whether or not the College member is in Ontario at the time. In other words, a member of the College of Psychologists of Ontario who is travelling outside of the province may provide services via technology to clients located in Ontario while they are away. Specific information about the provision of services via technology may be found in in Standard 15 of the Standards of Professional Conduct, 2017.
First, it is good to know that you are helping them to address these issues, as a colleague. It does not appear that you have a duty to report this situation.
There are two situations in which you may have a mandatory reporting obligation, but this does not sound like it is one of them. The two situations are set out in Section 85.2 and Section 85.5 of the Health Professions Procedural Code, being Schedule 2 of the Regulated Health Professions Act, 1991. The first applies to operators of facilities in which a health professional provides services:
Reporting by facilities
85.2 (1) A person who operates a facility where one or more members practise shall file a report in accordance with section 85.3 if the person has reasonable grounds to believe that a member who practises at the facility is incompetent, incapacitated, or has sexually abused a patient.
From your description of the situation, it doesn’t sound like you operate a facility in which this colleague practices, therefore this section would not apply.
The second relevant section of the Code applies to reporting by employers, etc.
Reporting by employers, etc.
85.5 (1) A person who terminates the employment or revokes, suspends or imposes restrictions on the privileges of a member or who dissolves a partnership, a health profession corporation or association with a member for reasons of professional misconduct, incompetence or incapacity shall file with the Registrar within thirty days after the termination, revocation, suspension, imposition or dissolution a written report setting out the reasons.
Same
(2) Where a member resigns, or voluntarily relinquishes or restricts his or her privileges or practice, and the circumstances set out in paragraph 1 or 2 apply, a person referred to in subsection (3) shall act in accordance with those paragraphs:
- Where a person referred to in subsection (3) has reasonable grounds to believe that the resignation, relinquishment or restriction, as the case may be, is related to the member’s professional misconduct, incompetence or incapacity, the person shall file with the Registrar within 30 days after the resignation, relinquishment or restriction a written report setting out the grounds upon which the person’s belief is based.
- Where the resignation, relinquishment or restriction, as the case may be, takes place during the course of, or as a result of, an investigation conducted by or on behalf of a person referred to in subsection (3) into allegations related to professional misconduct, incompetence or incapacity on the part of the member, the person referred to in subsection (3) shall file with the Registrar within 30 days after the resignation, relinquishment or restriction a written report setting out the nature of the allegations being investigated. 2014, c. 14, Sched. 2, s. 12.
Application
(3) This section applies to every person, other than a patient, who employs or offers privileges to a member or associates in partnership or otherwise with a member for the purpose of offering health services. 1993, c. 37, s. 23.
Once again it does not appear that you would have a reporting obligation unless you are the colleague’s employer and due to concerns of incapacity you terminated their employment or revoked, suspended or imposed restrictions on their privileges to practice or you dissolved a partnership, a health profession corporation or association with them.
Hopefully, with your collegial support, this individual will be able to mitigate the risks to themself and their clients and find relief from their distress. If it appears advisable for your colleague to obtain professional services, then you should consider referring them to an appropriate mental health professional, to avoid becoming involved in a dual relationship.
This is a situation that requires some definitional framing, before looking at the issue of feedback.
The Standards of Professional Conduct, 2017 define a “client” as:
an entity receiving psychological services, regardless of who has arranged or paid for those services. A client can be a person, couple, family or other group of individuals with respect to whom the services are provided. A person who is a “client” is synonymous with a “patient” with respect to the administration of the Regulated Health Professions Act (1991).
This means that the person who has been assessed is, from the perspective of the College, the client. Members are expected to be proactive in ensuring that clients are aware of their rights, including the right to access information about themselves, in accordance with the following Standard:
3.2 Clarification of Confidentiality and Professional Responsibility to Individual Clients and to Organizations
In situations in which more than one party has an interest in the psychological services rendered to a client or clients, members must, to the extent possible, clarify to all parties, prior to rendering the services, the dimensions of confidentiality and professional responsibility that must pertain in the rendering of services. The provision of psychological services on behalf of an organizational client does not diminish the obligations and professional responsibilities to individual clients.
Practical Application: The need for clarification may arise, for example, in the provision of an assessment of a claimant in an insurance matter, where the insurer has retained the assessor. Regardless of the wishes of the insurer, members are under all of the obligations that pertain to a client within these Standards and the relevant privacy legislation. This includes providing access to the individual or their authorized representative to their personal information and any reports or records which members have in their possession unless prohibited by law or they are otherwise permitted to refuse access.
The requirement to provide feedback, upon request by the client, is addressed in Ontario Regulation 801/93 Professional Misconduct:
The following are acts of Professional Misconduct:
…
13. Failing to provide a truthful, understandable and appropriate explanation of the nature of an assessment, intervention, or other service following a client’s request for an explanation.
…
21. Failing, without reasonable cause, to provide a report or certificate relating to a service performed by the member, within a reasonable time, to the client or his or her authorized representative after a client or his or her authorized representative has requested such a report or certificate.
Similarly, members are required to make information, including assessment results, available to all clients and authorized representatives, under the following Standard:
8.2 Access by Client or Client’s Authorized Representative
Members are responsible for ensuring that access to an individuals’ personal or personal health information is provided to the individual and/or their authorized representative unless prohibited by law or the member is otherwise permitted to refuse access.
While it may at first seem possible to find a technical “out” to providing feedback to someone who has not actually requested it, the Personal Health Information Protection Act, 2004 (PHIPA) specifies that consent to disclose information must be obtained from the person who has been assessed (or an authorized Substitute Decision Maker), and only if they have knowledge of the purposes of the disclosure. The consent must also be related to the information to be disclosed. In other words, there is a positive responsibility on the part of the Health Information Custodian to ensure that the client has been provided with an opportunity to make a free and informed decision about the disclosure of the information that would be disclosed.
There are two situations in which members have a duty to report incapacity-related concerns. These are set out are set out in Section 85.2 and Section 85.5 of the Health Professions Procedural Code, being Schedule 2 of the Regulated Health Professions Act, 1991. Neither of these appear to apply to a situation in which the concern regarding incapacity is with a client.
If you believe that this individual is putting members of the public at risk you can always make a report to the professional’s College, with their consent. In addition, Section 40 of The Personal Health Information Protection Act, 2004 also permits you to make a voluntary report, without the client’s consent, if you believe, on reasonable grounds that such a disclosure is necessary as they are putting clients at significant risk of serious bodily harm:
Disclosures related to risks
- (1) A health information custodian may disclose personal health information about an individual if the custodian believes on reasonable grounds that the disclosure is necessary for the purpose of eliminating or reducing a significant risk of serious bodily harm to a person or group of persons.
Section 13, specifically 13.2, of the Standards of Professional Conduct, 2017 requires members to responsibly assess their well-being and avoid impairment:
- Professional Objectivity
13.2 Compromised Objectivity, Competence or Effectiveness Due to Other Factors
A member must not undertake or continue to provide psychological services when personal, scientific, professional, legal, and financial or other interests could reasonably be expected to:
- a) impair his/her objectivity, competence or effectiveness in delivering psychological services; or
- b) expose the client to harm or exploitation.
Members are expected to use their professional judgement in considering their personal workload tolerance. The Quality Assurance Committee had developed a Self-Care Plan to provides some guidance in this area. The Quality Assurance Program requires that every member formally reflect upon their own need for self-care and mitigate the risk of harm to their own well-being and consequently that of their clients.
The College has not identified “parents” as a specific population to whom one needs particular authorization to consult to or otherwise work. The answer to your question then is: It depends upon the specific focus of the consultation.
If the parenting work involves psychoeducation, that is, providing parents with information about child development and advice about how they can address childhood difficulties, then it would make sense that a practitioner has been deemed to have the requisite knowledge, training, and experience required to understand the developmental factors at play with children/adolescents being ‘parented’. In this situation, authorization to work with children and adolescents would be expected.
If the focus of the work is to help parents improve their relationship with their child, then specialized knowledge, skill, and experience in the area of family dynamics is important. For this reason, authorization to work with families would be necessary.
Similarly, if the focus of the work is helping the parents work together as a couple, then authorization to work with couples, would be appropriate. Likewise, if the work involves assisting an individual parent who for personal reasons experiences challenges in interacting with a child and this requires them to receive individual therapy to address their own difficulties, authorization to work with individuals within that parent’s own age group would be required. Since you are authorized to work with adults, assuming that the parents are adults, then this would not be problematic.
Basically, one size can’t fit all, and the system of authorized populations allows for flexibility because of all of the possibilities with this kind of work.
Section 125 of the Child, Youth and Family Services Act, 2017 (CYFSA) sets out the duty to report a child in need of protection. It states:
125 (1) Despite the provisions of any other Act, if a person, including a person who performs professional or official duties with respect to children, has reasonable grounds to suspect one of the following, the person shall immediately report the suspicion and the information on which it is based to a society. Society is defined in the legislation as an agency designated as a children’s aid society under subsection 34 (1);
In considering this section of the legislation, there are two components to contemplate. First, there is nothing in the legislation which suggests that the suspected abuse or neglect must have occurred in Ontario to be reportable. Therefore, one is obligated to make a report regardless of where the suspected concerning behaviour occurred.
Second, the duty to report is to a “society” which the Act states is an agency designated by the Minister of Children and Youth Services as a children’s aid society. Since the Minister only has the authority to designate an agency as a “society” within Ontario, the obligation to report “to a society” must be to an appropriate agency within Ontario.
This analysis suggests that if a member has an obligation to report a suspicion of abuse or neglect which occurred outside of Ontario, they would have a duty to report to an Ontario CAS. It would then be up that agency to determine the best course of action to take but the member would have fulfilled their legislative obligation.
Section 125 also sets out the nature of emotional harm that a child must be experiencing, or which it is reasonably expected would experience, to necessitate a report, if the harm results from, or would be expected to result from the actions, failure to act or pattern of neglect on the part of the child’s parent or the person having charge of the child.
A: The Information and Privacy Commissioner of Ontario (IPC) recently addressed this issue in PHIPA DECISION 133, October 2020.
The Decision sets out the statutory limits to what one may charge, as follows:
[12] Under PHIPA, custodians have the discretion to charge a fee for providing an individual with access to their own personal health information. Sections 54 (10) and (11) state:
Fee for access
54 (10) A health information custodian that makes a record of personal health information or a part of it available to an individual under this Part or provides a copy of it to an individual under clause (1) (a) may charge the individual a fee for that purpose if the custodian first gives the individual an estimate of the fee.
Amount of fee
(11) The amount of the fee shall not exceed the prescribed amount or the amount of reasonable cost recovery, if no amount is prescribed.
The legislation does not prescribe an amount for “reasonable cost recovery”. In providing Reasons in Decision 33, the Adjudicator for the IPC states, previous IPC orders and PHIPA Decision 17 conclude that the 2006 fee scheme set out in the proposed regulation to PHIPA provides the best framework for determining the amount of “reasonable cost recovery” under section 54(11) of PHIPA.
| 2006 Fee Scheme | |
| Flat rate including: – 15 minutes of review – 20 pages of photocopies – packing and mailing the records – administrative tasks |
$30.00 |
| Photocopies or computer printouts after the first 20 pages | $0.25 per page |
| Review of the records after the first 15 minutes | $45 for every 15 minutes of review by a health information custodian after the first 15 minutes. |
The Decision provides a detailed analysis of the particular case and anyone facing this sort of issue is advised to read the entire Decision. For ease of reference, here is an excerpt from the Reasons that the Adjudicator gave for a finding that the health professional’s charges were excessive:
[44] In PHIPA Decision 111, I determined that not every type of record containing personal health information subject to PHIPA requires the same amount of time for review. … records with standard, predictable content require only a straightforward review with minimal time needed to determine whether they contain information to which access may be refused. For these types of records, I determined a review time of five seconds per page was appropriate. I found that other records, which by their nature, have the potential to contain information to which access may be refused, require a more detailed and lengthy review. For these types of records, I determined a review time of two minutes per page was appropriate… I have no evidence before me to suggest that any of the records at issue have the potential to contain personal health information that may required a more detailed and lengthy review…
[46] As a result, and in the absence of evidence to the contrary, in my view it is reasonable to conclude that the 27 pages of responsive records would require only a straightforward review at five seconds per page. Accordingly, I find that a reasonable amount of time for the custodian to review 27 pages of records containing the complainant’s own personal health information is encompassed in the first 15 minutes of review that are accounted for in the set fee of $30 per request. Given the nature and number of responsive records, I find that when the 2006 fee framework is applied, the custodian is not permitted to charge review fees in excess of what is accounted for in the set fee of $30. I accept that, in the circumstances, this amounts to “reasonable cost recovery” as required by section 54(11) of PHIPA.
While this reasoning is not enshrined in legislation or in formal guidelines, the precedent set by this, and previous Decisions should be considered by members when they set fees for the copying of records.
Although there are no specific requirements identified with respect to formal notetaking in a consultation relationship, there are specific requirements with respect to services to Organizational Clients. The Standards of Professional Conduct, 2017 define an Organizational Client as: an organization, such as a business, community or government that receives services that are directed primarily at the organization, rather than to the individuals associated with that organization.
If the social worker is thought of as operating a business, it is the business (as opposed to the social worker’s clients) to whom you are providing consultation. This would mean the records are Organizational Client Records. The Standards of Professional Conduct, 2017 set out the following requirements for Organizational Client records as follows:
9.3 Organizational Client Records
- Members must keep a record related to the services provided to each organizational client.
- The record must include the following:
- the name and contact information of the organizational client;
- the name(s) and title(s) of the person(s) who can release confidential information about the organizational client;
- the date and nature of each material service provided to the organizational client;
- a copy of all agreements and correspondence with the organizational client; and
- a copy of each report that is prepared for the organizational client.
Although the “nature of each material service provided” is not described, it can be reasonably understood that this means information about the issues discussed and advice given should be recorded. This would apply to any consultation, including those involving members of other professions.
The Standards of Professional Conduct, 2017 require that supervising members must be authorized to autonomously provide services to the specific populations before supervising others in that work. Furthermore, the Standards also requires that
Supervising members must assess the knowledge, skills and competence of their supervisee and provide supervision as appropriate to the supervisee’s knowledge, skills, and competence, based on this assessment;
Unless a supervisor has sufficient information about a client and the client’s difficulties, they would not be able to provide adequate supervision appropriate to the supervisee’s knowledge, skills and competence.
It is the responsibility of a supervisor to be sufficiently familiar with the client’s demographics and needs before permitting their supervisee to commit to provide services. The adequacy of the supervision could be in question if a supervisor reviews and signs off on reports without having been involved in a direct or supervised intake process, or does not actively supervise the work leading up to any final reports.
Even though the Standards do not require supervisors to meet and interact with clients receiving services under their supervision, a supervisor should only permit a supervisee to work with a client after they have satisfied themselves that the client is within their authorized areas of practice and belongs to a population with whom they are authorized to work.
The Definition of Practice Areas are published as part of the Registration Guidelines. Within the Guidelines, the definition of Counselling Psychology stresses fostering and improving human functioning by helping individuals solve problems, make decisions and cope with stresses of everyday life. These can include work/career/education, family and social relationships, and mental health and physical health concerns. In other words, these are the types of difficulties which may cause distress to an otherwise well-functioning or psychologically healthy individual. Some common examples of such problems are bereavement, unemployment, marital separation, or bankruptcy, etc. Generally, an individual presenting as having a disorder of behaviour, emotion or thought, should be assessed and treated by a member authorized in Clinical Psychology.
As described in the Definition of Practice Areas, members who practice Counselling Psychology, at a minimum, are expected to have « the ability to formulate and communicate a differential diagnosis in order to develop an appropriate counselling intervention and to identify clients who must be referred elsewhere”.
In contrast to that of Counselling Psychology, the definition of Clinical Psychology, as described in the Definition of Practice Areas, is « the application of knowledge about human behaviour to the assessment, diagnosis and/or treatment of individuals with disorders of behaviour, emotions and thought”.
It is sometimes unclear at the initial stages of involvement whether a client has a “disorder”, and this is an important reason that those authorized in Counselling Psychology be able to perform a differential diagnosis. When a client presents with indicators of a disorder of behaviour, emotion or thought, a member who is not authorized in Clinical Psychology should refer them to a member authorized in this area.
If, at the time of referral, an individual presents with indicators that suggest they may have a diagnosable disorder, it would be most appropriate for an assessment to be conducted by someone qualified to work with those with clinical disorders. One should carefully consider the implications of beginning to work with someone that is likely to need to be transferred to someone else’s care. This could be quite disruptive to the client and the clinical relationship, and may even be damaging to their well-being and/or treatment.
At times, the extent of a client’s difficulties may not be apparent at the initiation of services, and it may later become evident that the client is suffering from a clinical disorder. If a member, authorized in Clinical Psychology, is not available to accept a referral, it would be permissible to obtain supervision from someone so authorized. This should be considered a “last resort” however, and not a “workaround” for appropriate authorization.
It is appropriate for private practitioners, including contractors, to be compensated based on time spent and the complexity of services provided. If providing additional incentives to treatment providers could be reasonably expected to lead to decisions about service planning that are motivated by factors beyond client needs this could be problematic. For example, this could be problematic if compensation rather than client needs lead to practicing the profession while in a conflict of interest and/or providing services which are not likely to benefit the client; both of which are considered acts of Professional Misconduct. Members are advised to support their staff and contractors in ensuring that client need is the primary consideration in service planning.
We’ve heard about this incorrect position from enough people to assume that, at some time in the past, it must have been promulgated widely. While the legislation permits one to refuse access to personal health information in some limited circumstances, including raw data from psychological tests, it does not prohibit one from allowing access to it. In many cases, it is expected that raw data will be provided, even with non-members.
A list of exceptions to the right of access to personal health information can be found in section 52 of the Personal Health Information Protection Act (PHIPA), 2004. Most of the exceptions relate to the expectation of serious risk associated with the disclosure.
Members who have insufficient cause to withhold raw data may have concerns about the risk of releasing the information to those who are not sufficiently trained to interpret it. In such cases, members are advised to attach a statement to the raw data indicating that raw data from standardized tests can lead to incorrect conclusions, and that this information should only be interpreted by those who are regulated psychological service providers with adequate training and experience in the interpretation of test results.
Detailed further information about the release of raw data can be found on the College’s Professional Practice FAQ pages.
As required by Standard 4 of the Standards of Professional Conduct, 2017, members supervising anyone who is not a member of the College and any member with a Certificate of Registration Authorizing Supervised Practice must co-sign all psychological reports and formal correspondence related to psychological services prepared by their supervisee.
The term “formal” has not been officially defined so members must use their professional judgment based upon the particular circumstances of each situation.
In generally, formal documents would likely include printed or electronic communications which ordinarily require the person responsible for the information to provide their endorsement of the information in the form of a signature. This might include letters, reports, official memos, and emails about a client which would reasonably be expected to provide information about a client to anyone outside of the organization in which the supervision is occurring.
When in doubt about whether to co-sign a document, it may help to consider that a supervisor’s signature is meant to provide an assurance to readers of the information it has been endorsed by the professional responsible the service. Even if not strictly required to co-sign a document, supervising members may do so if they wish to inform readers that they endorse the contents.
It is a client’s right to decide who their personal health information may be shared with, subject to some exceptions set out in the Personal Health Information Protection Act (PHIPA), 2004. The Office of the Information and Privacy Commissioner of Ontario has published some helpful information about the Circle of Care, a colloquial term describing how one may rely on implied consent and the Lock Box, the colloquial language used to describe how a client may limit what can be shared where one could ordinarily have relied upon implied consent. All members who have not yet reviewed these documents, should familiarize themselves with these concepts and rules.
While there may be an argument that a member is not technically violating PHIPA if they provide information based upon implied consent, it isn’t really in the spirit of the legislation to do so, particularly if one believes a client who understood their rights, might capably choose to limit disclosure of their personal health information.
If there is reason to believe that a client would not want their personal health information shared, even if they have not sought to have the information ‘placed in a lock box’, one should consider the impact of sharing the information on the therapeutic alliance or on the client’s trust of other health care professionals, if the client believes their privacy has not been respected.
This question has been answered by the Office of the Information and Privacy Commissioner of Ontario and can be found in the Frequently Asked Questions; Personal Health Information Protection Act September 2015, on page 31 of the document.
The answer reads as follows:
Yes. PHIPA permits the disclosure of personal health information without consent, if permitted or required by another law. For example, this means that PHIPA does not interfere with the Workplace Safety and Insurance Act (Act), where that Act requires a hospital or health facility, which provides health careto a worker claiming benefits under the insurance plan, to give the WSIB such information relating to the worker as the WSIB may require. This requirement also applies to a health care practitioner who provides health care to a worker or is consulted with respect to a worker’s health care. When requested to do so by an injured worker or the employer, the Act requires a health care practitioner treating the worker to give the WSIB, the worker and the employer prescribed information concerning the worker’s functional abilities.
The Standards of Professional Conduct directly address the use of technology in the generation of assessments, reports and statements:
10.7 Use of Computer-Generated Reports
Information obtained from computer-generated assessments, reports or statements must not be substituted for a members professional opinion.
Members are free to responsibly use technological advances as an adjunct to their own assessments and interventions, however, it is the position of the College that these professional activities must always be actively mediated by members who are authorized to provide the services and that members must remain fully accountable for services provided in their names.
To date, there is insufficient scientific evidence to demonstrate the effectiveness and safety of using ChatGPT or other Artificial Intelligence (AI) to assess or treat mental health conditions and the risk to clients may outweigh any potential benefits. Anyone considering the use of AI to assist or augment their services should ensure, as part of the informed consent process that clients understand how technology is being used to assist them, what the risks are of technological error, and also what risks there are to their privacy when personal information is being used in an AI context.
The answer to this question depends upon the reason for involving family members in the treatment of an individual.
Individual therapists appropriately may involve a client’s family member(s) for the purpose of facilitating support for intervention with the individual. For example, a person’s family member(s) might be asked to become involved in making changes in the client’s environment to facilitate change or to be trained to provide reinforcement for desirable behaviours as part of a behavioural intervention program. A family member could also be asked to attend sessions with a person who, for some reason, may not be able to successfully participate in individual therapy without support. In such a scenario, the family member(s) attending would not be the object of the intervention themselves but would instead be there to help the client obtain optimal benefit from the individual therapy.
If the purpose of involving family members is to facilitate any changes in the family dynamics or the way in which family members interact with one another, this would be viewed as an family intervention. For example, this would be the case when it is the therapist’s intention to address an individual’s symptoms or behaviours of concern by addressing the patterns of interaction between family members which precipitate or maintain the difficulties. In order to provide such intervention to families, one must have specialized knowledge and training and the specific authorization of the College.
Originally published in Volume: 1 Issue: 1 of HeadLines.
In Ontario, there is no duty to warn, if one interprets “duty” to mean a mandatory requirement. That is, there is no obligation to report concerns that a client/patient may pose a danger to themselves or others. It is important to understand however, that this does not mean that one cannot, or should not, take some action in the face of such serious concerns. The Personal Health Information Protection Act, 2004 (PHIPA) sets out a member’s obligations with respect to maintaining the confidentiality and privacy of personal health information. The legislation does provide an exception to the duty of confidentiality where a member finds it necessary to notify someone of a serious risk to a person’s safety. PHIPA states:
40 (1) A health information custodian may disclose personal health information about an individual if the custodian believes on reasonable grounds that the disclosure is necessary for the purpose of eliminating or reducing a significant risk of serious bodily harm to a person or group of persons. 2004, c. 3, Sched. A, s. 40 (1).
A key concept within this section of PHIPA is contained in the words “may disclose”. PHIPA does not oblige a member to make such disclosures, but it permits one to do so “for the purpose of eliminating or reducing a significant risk of serious bodily harm”. With this purpose in mind, PHIPA reinforces a member’s need to use their knowledge of the client/patient and their professional judgement to determine the best, most appropriate, action to take.
With the relaxation of pandemic-related restrictions on in-person services, some members are exploring whether to return to in-person service delivery or to continue providing all services virtually. There is no specific prohibition against offering online services.
Members must use their professional judgment in deciding whether to offer in-person vs. virtual services, taking into consideration the needs of each individual seeking services and the available evidence regarding efficacy.
Members are expected to provide services in a safe and effective manner. If a member wishes to restrict their practice to virtual services, they must decide which populations and problem areas can be effectively assisted without in-person contact, and under what circumstances this would be appropriate.
There is no ‘one size fits all’ when it comes to planning service delivery in psychology. It may be that some clients are more comfortable with on-line services and might be more likely to engage in services provided via technology and some intervention models may lend themselves to on-line delivery more than others. Members should also consider some concerns that have been raised about services delivered via technology. These include:
• loss of many visual cues and other sensory inputs which are less accessible via the computer screen or telephone than when physically present with a client;
• increased risk to breaches of confidentiality;
• increased need for vigilance concerning professional boundaries and personal privacy; and
• issues of equity, as some clients will not have access to technology, sufficient familiarity and/or competence in using it, and/or the necessary adequate privacy.
Members providing virtual care must adhere to all of the Standards of Professional Conduct, 2017 including, but not limited to, Standard 15, Use of Technology in the Provision of Psychological Services. An additional resource members may find useful is the American Psychological Association’s Guidelines for the Practice of Telepsychology. This is a helpful guide in reflecting upon the delivery of services via technology. Some of the areas addressed in the article are the need to: regularly monitor and assess the progress of the client/patient to determine if the continued provision of telepsychology services remains appropriate and beneficial; discuss any concerns with the client/patient; and appropriately terminate remote services and provide assistance in arranging alternative services, if necessary.
If a member initially agreed to provide in-person services to a client; transitioned to on-line services during the pandemic; and wishes to continue with on-line services beyond the point at which it seems necessary, this can be problematic if the client wishes to return to in-person services. In such a situation, a member may decide to terminate services against a client’s wishes, but should be mindful of the section 1.8 of O. Reg. 801/93: Professional Misconduct Regulation which sets out the manner in which one can do so that would not be considered professional misconduct.
Originally published in Volume: 1 Issue: 1 of HeadLines
The legislation does not direct a member to contact any particular organization, institution or individual should it be determined there is a need to take some action. In considering a breach of confidentiality under section 40 of PHIPA, it is important that, in keeping with the stated purpose, the disclosure be made to someone who is in a position to ‘eliminate or reduce a significant risk of serious bodily harm’.
When faced with serious concern about a client’s/patient’s risk of harm to self or others, members have to make the difficult judgment about who to contact in this time of crisis. When initially reviewing the limits of confidentiality regarding risk of harm with a client/patient, members may wish to discuss this with the client/patient. That is, engage the client in a discussion of who they believe should be called in the event of a crisis. The client/patient may identify a family member, other health care provider, close friend, member of the clergy, a community worker, an organization with which they have been involved or some other individual. While the ultimate decision rests with each member based on their best clinical judgement, taking into account their understanding of the client/patient and the particular situation, this previous discussion may prove helpful in deciding upon the most appropriate action.
It is important to make a distinction between situations of client/patient risk of harm to themselves or others, often referred to as “duty to warn” and other mandatory reporting obligations. Section 40 of PHIPA does not apply to situations where one has reasonable grounds to suspect that a child is in need of protection or one suspects abuse or neglect in a retirement or long-term care facility. In these situations, mandatory reporting to the appropriate authority is required.
The answer to this question requires interpretation of legislation and College staff are not qualified or authorized to provide legal advice. Members who are considering refusal of a specific request for information may wish to obtain independent legal advice, given that release of confidential information, or the refusal to do so, can be a high-stakes decision for all concerned. The following information may be of assistance in obtaining legal consultation.
The Personal Health Information Protection Act, 2004 (PHIPA) sets out the applicable rules to be considered when addressing a request for personal health
information.
Personal Health Information is defined, in section 4.(1)(a) of the Act, as information that “relates to the physical or mental health of the individual, including information that consists of the health history of the individual’s family. . .”
Section 1 (b) of PHIPA states that one of the purposes of the Act is “to provide individuals with a right of access to personal health information about themselves, subject to limited and specific exceptions set out in this Act”. The Act also provides that information an individual is entitled to access can be provided to another party, with the consent of the individual or of the individual’s authorized substitute decision-maker.
Whenever faced with a decision about whether to provide access to information contained in a client record, it is a good idea to review the list of exceptions to the requirement to do so. These exceptions are set out in in Section 52(e) of the Act where one is not required to allow access to information if,
(e) granting the access could reasonably be expected to,
i. result in a risk of serious harm to the treatment or recovery of the individual or a risk of serious bodily harm to the individual or another person,
ii. lead to the identification of a person who was required by law to provide information in the record to the custodian, or
iii. lead to the identification of a person who provided information in the record to the custodian explicitly or implicitly in confidence if the custodian considers it
appropriate in the circumstances that the identity of the person be kept confidential;
The Act, section 52(2) goes on to say that a health information custodian may provide only parts of a person’s record “that can reasonably be severed from the part of
the record to which the individual does not have a right of access”. When a decision is made to sever part of a file before releasing the record, section 54 of the Act provides
specific guidance about how to do this.
The Information and Privacy Commissioner of Ontario recently considered a complaint about an agency’s refusal to grant one family member access to the entirety of a family’s therapy records. In PHIPA Decision 158, the Commissioner found that the Personal Health Information (PHI) of each family therapy participant is theirs alone and not PHI of the other therapy participants. They went on to say that family therapy records may contain “communal” or “shared” information that can form part of each participant’s PHI. Communal or shared information was described as information about family health history, overall family relationships or dynamics, as well as general themes that arose in the course of family therapy.
The Commissioner ultimately decided that the complainant’s right of access under PHIPA was limited to only to PHI that can reasonably be severed from the records. The Decision explains that the Act is intended to enable individuals to access information about their family health history allowing them to make informed decisions about their own health care but that anything beyond shared or communal information, may have been collected with an expectation that it would remain confidential.
The Decision further explained that this best respects the confidentiality of that information; fosters trust between family therapy participants and custodians; promotes participant autonomy over access to their own personal health information; and promotes candid discussion and unguarded participation in family therapy sessions.
The Decision indicated that the right of access to information is limited by section 52(3), of the Act, which provides that an individual will only have a right of access to an entire record if the record is “dedicated primarily” to their personal health information. The following examples of factors to consider in determining whether a record is “dedicated primarily” to the personal health information of a requester are provided:
- the quantity of personal health information of the requester in the record;
- whether there is personal health information of individuals other than the requester in the record;
- the purpose of the personal health information in the record;
- the reason for creation of the record;
- whether the personal health information of the requester is central to the purpose for which the record exists; and
- whether the record would exist “but for” the personal health information of the requester in it.
The following “best practices” are suggested within the Decision:
- At the outset of therapy, establish ground rules for what can be discussed, what information will be recorded, and who will have access to the records;
- Document this understanding in the health record;
- Identify documents (including chart notes) that relate to one participant and those that relate to all participants; and
- When considering requests to access family or group therapy records, refer to documented informed consent and other records to identify participants’
expectations, and categorize records as communal or relating to one or more participants before granting access to any records.
Originally published in Volume: 1 Issue: 2 of HeadLines
The College doesn’t specify hard borders between age ranges for the different population groups but recognizes that there are not always clear demarcations with respect to population groups, particularly with respect to age. Members are expected to use their professional judgment to determine whether, in all the circumstances, the person’s status is consistent with the status of those for whom they are authorized to provide service. For example, when trying to determine whether a client, at a border age, is an “adult”, “adolescent”, or for that matter a “senior”, it would be important to consider whether the person’s abilities, life circumstances and challenges are consistent with those which would normally be expected within the population groups for which the member is authorized to work.
Originally published in Volume: 1 Issue: 2 of HeadLines
As members know, the College has defined Authorized Areas of Practice. The definitions for the authorized areas of practice focus on the nature of difficulties the services are intended to address, as opposed to the specific type of service offered. In order to answer questions like this it may be most helpful to keep this distinction in mind.
The Practical Application posted with Standard of Professional Conduct, 2017 5.1 states: In deciding whether one is authorized and competent to provide a service, the nature of the client’s presenting difficulties will generally determine whether the member has the appropriate and required authorization. For example, if a client who has suffered a traumatic brain injury has been referred because of a need to assess the nature of their neuropsychological deficits, it is expected that the member providing the assessment would have clinical neuropsychology as an authorized area of practice. If the person was referred because of difficulty performing activities of daily living or occupational requirements, it is expected that the member would be authorized to work in the area of rehabilitation psychology. If the person was referred because of suspected anxiety or depression, then it is expected that the member would be authorized to practice in clinical psychology…
It’s likely that most of what are often called “psychoeducational assessments” are meant to help identify the reason an individual has difficulty learning in an educational environment and to provide information for the purpose of planning for remediation of these difficulties. If there is reason to believe that the nature of difficulties is neuropsychological in nature, then it would appear reasonable for someone with authorization in the area of Clinical Neuropsychology to assess the client.
At the same time, authorization in School Psychology requires certain knowledge not generally required for the practice of Clinical Neuropsychology, including knowledge of:
- academic, instructional and remedial techniques;
- interdisciplinary team approach for case management, program planning and crisis intervention;
- consulting, counselling, and primary, secondary and tertiary intervention programs and techniques;
- systems and group behaviours within, and related to, the school organization, including school climate and culture.
If making specific recommendations which require such knowledge, it’s expected that a member who has not acquired this knowledge would seek the professional guidance of another member who is authorized to practice School Psychology.
Originally published in Volume: 1 Issue: 2 of HeadLines
Members may provide services to an individual located in another jurisdiction, but only if they have been authorized by the College or Board in that jurisdiction to do so. If the psychology regulator in the other jurisdiction permits this practice, it would also be important to confirm that one’s professional liability insurance coverage extends to one’s work with an individual in the other jurisdiction.
Originally published in Volume: 1 Issue: 3 of HeadLines
The Professional Misconduct Regulation and Standards of Professional Conduct, 2017 do not specifically address the issue of whose name to put on an invoice. Therefore, one must ensure adherence to the broader rules when deciding about how to proceed regarding what information to put on an invoice or receipt. The most important thing is to ensure is that any document, including an invoice or receipt, could not reasonably be seen as, 20. Making a record, or issuing or signing a certificate, report, or similar document that the member knows or ought to know is false, misleading or otherwise improper. [O.Reg 801/93 Professional Misconduct]
In cases where multiple members of a family are treated at different times and in different constellations, it would be reasonable to make a principled decision and apply the same logic whenever similar situations arise, regardless of the wishes of the particular client or what their insurance coverage allows.
In this particular case, if an intervention is intended to impart parenting skills to the parent, it might be reasonable to assume that parenting work is intended to help the parents change their behaviour and consider that the services were provided to the parents. This would be different than meeting with the parents in order to provide them with therapy progress information or information to help them support the work being done individually with the child.
Most of the time this question comes up in the context of a family with per-person insurance coverage limits. In situations like this, a parent may ask to revise invoices or receipts once a family member reaches their insurance coverage limit. One must be careful not to issue an invoice in a manner where it could be alleged that the person issuing the invoice was participating in something that could be seen as misleading.
Wherever possible, it might be helpful to ensure an invoice provides clear information about the nature of service and identifies those to whom the service was provided. If a person to whom the service was provided is different than the person who is the focus of the treatment, it may be appropriate to note on the invoice something like services were provided to Mr. and Mr. Smith re: the treatment of their child James Smith. Clients may also be asked to consult with their benefits providers about how to best maximize their coverage and the insurer’s preferences with respect to billing.
While it may feel helpful to assist clients in maximizing their insurance coverage, insurers are becoming increasingly vigilant about such matters and this could result in denial of benefits to the client and a complaint to the College. It should be left to the client(s) and their insurers to work out issues about insurance coverage limits.
Originally published in Volume: 1 Issue: 3 of HeadLines
This scenario presents some potential challenges.
Consent may be more complicated than might initially meet the eye. The clients in such a situation could decide to enter the relationship because of a perceived expectation by the therapist that they will agree and not want to disappoint the therapist by declining the invitation. For this reason, if this were to occur, such an opportunity would have to be presented in an entirely neutral manner.
To be fully informed consent, each client would have to be made aware of all the potential benefits and risks. These benefits would obviously include mutual support. On the downside, entering a relationship in which the client could be taking on further emotional (and perhaps other) demands should be presented as a risk to their own therapeutic relationship with the therapist and consequently to their therapeutic progress.
Confidentiality could also become a challenge when clients are introduced and encouraged to communicate. While each client would know that the other was seeing the same therapist, the therapist would have to be vigilant not to share any information about the other client without authorization. This would become difficult if they wished to talk about the other client or about interventions being used with them and it could become difficult to avoid inadvertently providing information, even in refusing to actively answer certain questions that could be posed. Even if information about one client was never disclosed to the other, the therapist would have to be vigilant about avoiding the collection of information about one from the other without consent. Even with full consent, collection of such information could pose challenges to professional objectivity, if information arose about any conflict arising between these individuals or any adverse information about them. This would become a dual relationship in the same way as working with clients who are relatives or friends of one another would, and it’s best to avoid dual relationships.
There are no specific prohibitions against introducing clients, but these are some of the challenges in managing such an intervention, without the safeguards of therapist mediated interaction between clients, as might occur in a therapist mediated mutual support group.
Originally published in Volume: 1 Issue: 3 of HeadLines
A member of the College with a Retired Certificate of Registration or a former member may not provide any psychological services of any kind. They would however, be able to provide information regarding services provided while holding a Certificate of Registration Authorizing Autonomous Practice. If, for example, the court required the client to be reassessed or needed testimony about matters not addressed while the member held a Certificate of Registration Authorizing Autonomous Practice, this would appear to be a new service and not one that should be provided unless one is authorized to provide psychological services.
The College is not in a position to require, and assure the public, that members with a Retired Certificate of Registration are maintaining their professional competence through continuing professional development. They are also not required to maintain their professional liability insurance coverage, which protects clients who may have a legitimate claim for financial awards as a result of a member’s professional activities. This is obviously also the case for retired members as well.
Originally published in Volume: 1 Issue: 4 of HeadLines
This question often arises when a member has been treating or assessing a client where the primary focus of clinical attention has not involved an assessment of the factors bearing upon the opinion being sought. This may occur, for example, when a member has conducted a psychoeducational assessment, or treatment for an anxiety disorder, and the member is later asked to provide information to be used in a parental rights matter. Another example is when a member has provided psychotherapy to address a client’s emotional disorder and is then asked to provide a letter regarding the individual’s readiness to return to work after an injury.
In providing professional opinions, a member must consider the following requirement in section 10.3 of the Standards:
10.3 Rendering Opinions
A member must render only those professional opinions that are based on current, reliable, adequate, and appropriate information.
In the first example above, a member should only provide information that they can reasonably expect to be used to determine custody or access arrangements if they have conducted an appropriate assessment for the purpose of determining child custody and/or access. Likewise, in the second example, a member should only opine on a person’s suitability to return to work after appropriate consideration of the person’s rehabilitation needs and the task requirements of the workplace.
Members must ensure that they work only within their authorized areas of practice and provide only those services in which they have the adequate knowledge, skill, and experience, within those authorized areas.
Even when a member is authorized and qualified to provide an opinion unrelated to the service they have been providing, and have conducted an adequate assessment, problems may arise if they assume a dual role. Usually, such requests for information are related to the rights and entitlements of the client. They also have an impact on others, such as family members, colleagues, or employers. A clinician who has not conducted an appropriate, objective assessment of the matter at hand can face challenges with respect to whether they have exercised sufficient neutrality. There may also be a perceived conflict of interest if it appears that a continued professional relationship could be endangered by offering an opinion that is seen to be unfavourable to the client’s interests.
Originally published in Volume: 1 Issue: 4 of HeadLines
Section 4.1.1 of the Standards of Professional Conduct, 2017 requires that:
8) the supervising member must ensure that billing and receipts for services are in the name of the supervising member, psychology professional corporation or employer and clearly identify the name of the supervising member and the name, relevant degrees and professional designations of the supervised psychological service provider
There is no explicit requirement under this Standard for there to be a signature, however, the following Standards are also applicable to these situations:
4.1.2 Supervision of Supervised Practice Members; and
4.1.3 Supervision of Non-Members
In addition to the responsibilities outlined in 4.1.1:
a) the supervising member must co-sign all psychological reports and formal correspondence related to psychological services provided by non-member supervisees;
Invoices (and receipts) would be considered by most to be “formal correspondence” and should be co-signed by supervisors.
Within the past few years, the College has received an increasing number of complaints about the transparency of such documents and what some third-party payers have alleged to be misleading practices by members. Increasing vigilance by third-party payers has, unfortunately, led to denial of insurance benefits for some clients. It has also led to an increased level of scrutiny of College members by claims adjusters. Supervisors should demonstrate that they carefully oversee the administration of their services by personally applying their own signatures to invoices issued in their names.
Originally published in Volume: 1 Issue 4 of HeadLines
In determining the appropriate record keeping requirements it’s important to consider what is meant by “consultation”. Sometimes, those using the title “consultant” are actually providing direct services to individuals. For example, this would be the case if the service involved interviewing clients of an agency and providing an assessment of their treatment needs. The member would, in such a situation, be required to create a client record in accordance with section 9.2 of the Standards of Professional Conduct, 2017. Even if, by virtue of the administrative arrangements, the client is also a client of the agency and agency is the Health Information Custodian, the definition of client in the Standards is applicable:
Client: an entity receiving psychological services, regardless of who has arranged or paid for those services. A client can be a person, couple, family or other group of individuals with respect to whom the services are provided. A person who is a “client” is synonymous with a “patient” with respect to the administration of the Regulated Health Professions Act (1991).
If involvement in a case was limited only to discussing the client with the clinician providing the direct client care, it is more likely that the consultation met the definition provided in the Standards: Consultation: the provision of information, within a relationship of professionals of relatively equal status, generally based upon a limited amount of information that offers a point of view that is not binding with respect to the subsequent professional behaviour of the recipient of the information.
If acting as a consultant, as it is defined above, then the following requirements regarding contents of records apply:
9.3 Organizational Client Records
- A member must keep a record related to the services provided to each organizational client.
- The record must include the following:
a) the name and contact information of the organizational client;
b) the name(s) and title(s) of the person(s) who can release confidential information about the organizational client;
c) the date and nature of each material service provided to the organizational client;
d) a copy of all agreements and correspondence with the organizational client; and
e) a copy of each report that is prepared for the organizational client.
Even though the phrase “nature of” each material service, is not defined above, most prudent members record enough information to indicate the nature of the problem discussed and the nature of advice given.
Standard 9.4 provides the record retention requirements with respect to organizational records:
2) The organizational client record must be retained for at least ten years following the organizational client’s last contact. If the organizational client has been receiving service for more than ten years, information contained in the record that is more than ten years old may be destroyed if the information is not relevant to services currently being provided to the client.
Normes de Conduite Professionnelle 2017
The Standards of Professional Conduct, 2017 state that:
11.1 Fees and Billing Arrangements
Members must reach an agreement with an individual, group or organization concerning the psychological services to be provided, the fees to be charged and the billing arrangements prior to providing psychological services. Any changes in the services to be provided must be agreed to by the client before service is delivered or fees are changed. Fees must be based on amount of time spent and complexity of the services
rendered.
Practical Application: Fees for services should be determined on a consistent basis, regardless of the payer. A member may, however, offer pro bono services or apply a sliding scale to ensure access to services and affordability.
While this Standard is most often thought of in the context of initiating services with a new client, it also can be read to apply with respect to the ongoing provision of services. That is, “providing psychological services” could be read to mean each instance of providing a psychological service. It would be inappropriate for a client to learn that their fees had been increased when they receive a bill for a service that had already occurred. Increased fees may be an important consideration for clients in the ongoing informed consent to service process and some clients may need to reconsider whether they are able, or prepared, to continue at the new proposed rate.
There is no specific period of notice for a fee change set out in any Regulations or in the Standards as this is a matter of professional judgment. Adequate notice of the change however, is important and there may be clients who experience a fee increase as akin to indirect termination of therapy.
In cases where the client may not agree to an increased fee, and a member is not prepared to continue to provide services at the existing rate, guidance regarding the termination of services can be found in section 8 of O.Reg. 80.1/93: Professional Misconduct. This section of the Regulation states that termination of service that is needed is an act of professional misconduct unless:
i. the client requests the discontinuation,
ii. the client withdraws from the service,
iii. reasonable efforts are made to arrange alternative services,
iv. the client is given a reasonable opportunity to arrange alternative services, or
v. continuing to provide the services would place the member at serious personal risk.
Although there are informal ‘rules of thumb’ with respect to ‘winding down of therapy’, often based upon the length of time a person has been receiving treatment, the College does not set any particulars in this regard. If the client requires additional services but can not or will not pay the increased rate, it would be reasonable and appropriate to work with them for a time period that, in the member’s professional judgment, is sufficient to arrange for a transfer of care to another service provider and avoid any harm due to a disruption of treatment.
Introduction
The College has received many questions from members of the College and the public about the Controlled Act related to Psychotherapy since it was proclaimed on December 30, 2017.
Members of the College of Psychologists are permitted to perform the Controlled Act related to Psychotherapy, so members need not be concerned whether psychotherapy they provide falls within the definition of the Controlled Act. As always, members are responsible to ensure that they are competent to provide any psychological service they offer. The definition of when services fall within the Controlled Act becomes much more important when one is considering supervising someone in the performance of the Controlled Act.
Information currently available on the College website may address some of the member inquiries. This can be found in the Practical Applications to the Standards of Professional Conduct, 2017 in the Standards of Professional Conduct.
Further information is available and in the Questions and Answers document accompanying the Standards
The following information is intended to address the most frequently asked Questions the College has received. If there are other questions, you please email them to practiceadvice@cpo.on.ca.
Definitions
The Controlled Act related to Psychotherapy is defined in section 27(2) of the Regulated Health Professions Act, 1991 (RHPA) as:
14. Treating, by means of psychotherapy technique, delivered through a therapeutic relationship, an individual’s serious disorder of thought, cognition, mood, emotional regulation, perception or memory that may seriously impair the individual’s judgement, insight, behaviour, communication or social functioning.
The legislation does not define the terms used in this definition particularly “psychotherapy” and what is meant by “serious”. Within the Psychotherapy Act, 2007 however, the ‘practice of psychotherapy’ is defined as:
3. the assessment and treatment of cognitive, emotional or behavioural disturbances by psychotherapeutic means, delivered through a therapeutic relationship based primarily on verbal or non-verbal communication.
The legislation does not define “serious” with respect to what is a “serious disorder . . . that may seriously impair”. This is left to the treatment provider to apply his/her own education, skill, and training to determine. As noted above, this need not be of concern to members personally offering psychotherapeutic services as members of the College are authorized to perform this Controlled Act. It is important, however, when one is considering providing supervision. In the absence of any available jurisprudence defining these terms within the definition, especially as related to a “serious disorder . . . that may seriously impair” members of the College are expected to exercise their professional judgment in deciding whether the services which they contemplate supervising constitute the Controlled Act.
Whether an activity constitutes the Controlled Act requires consideration of the level of difficulty and potential impairment experienced by the client and is not dependent on a specific diagnosis or therapeutic modality.
Members who are not comfortable exercising their own professional judgment in deciding whether a service falls within the “serious disorder . . . that may seriously impair” definition of the Controlled Act should consult with another member, another regulated colleague authorized to perform this Controlled Act or seek legal advice.
Questions and Answers
1. Is the provision of all “psychotherapy service” now controlled by the new legislation?
No. As noted in the definition, only psychotherapy delivered to a client with a “serious disorder . . . that may seriously impair” their functioning falls within the Controlled Act.
2. In general, under what circumstances may I supervise the performance of the Controlled Act?
Most of the concerns raised are related to supervision by College members of others who are performing the Controlled Act. The RHPA specifically sets out that a person who is not yet authorized to perform the Controlled Act independently may do so under supervision but only if she/he is fulfilling the requirements to become a member of a health profession, the act is within the scope of practice of the profession and is done under the supervision or direction of a member of the profession [emphasis added].
It is important to note that College members may continue to supervise individuals they believe have the competence to provide psychotherapeutic services when those services fall outside of the Controlled Act.
3. With regards to performing the Controlled Act of psychotherapy, may I supervise:
a) Doctoral psychology students in practica or internship placements or individuals is in the process of obtaining their four years of supervised experience necessary to apply to become a psychological associate?
The legislation permits one to supervise individuals who are fulfilling the requirements of our College. This includes supervised practice members, students in practica or internships as well as those gaining their required post-masters experience.
b) Autonomous practice members of the College who may require supervision to expand their authorized areas of practice or their authorized population groups or who require supervision pursuant to a decision of the Inquiries, Complaints and Reports Committee (ICRC) or Discipline Committee?
Yes. Given that one is permitted to supervise a Supervised Practice member as noted above, it would seem inconsistent with the intention of the legislation for members not to be able to supervise another autonomous practice member to meet College requirements to practice in specific areas or with specific populations or fulfill a condition required by the ICRC or Discipline Committee.
c) Autonomous practice members of the College who may wish to increase their psychotherapy skills within their authorized areas of practice or their authorized population groups?
Generally, these members would become involved in a mentorship, consultation or training relationship, rather than a formal supervisory one. Since they are already authorized in the area or with the population, the College does not require supervision when a member is learning new techniques or increasing the scope of their activities within their authorized areas.
d) Individuals who are in the process of becoming a member of the College of Registered Psychotherapists of Ontario (CRPO) or another College whose members are authorized to perform the Controlled Act, but are not yet members of that College?
On December 21, 2017, the Minister of Health and Long-Term Care announced that, “Individuals who provide these services [the controlled act] will have a two-year transition period, beginning December 31, 2017, to register with a regulatory college.” Therefore, supervision of individuals in the process of becoming a member of the CRPO or another College whose members are authorized to perform the Controlled Act is permitted as follows:Transition Period to December 31, 2019:
The transition period appears to permit individuals to perform the controlled act whether or not they are under supervision. In keeping with the apparent intention of the transition period, that is to provide an opportunity for individuals to register with a relevant regulatory College; the College is of the view that it would be appropriate to permit members to supervise individuals who are preparing to become a member of the CRPO, during the transition period.It is important to note that there is no restriction with regard to College members offering training, support, consultation and mentorship to other practitioners. While the CRPO may use the term “supervision” in their requirements for candidates, their use of the term may connote a less formal arrangement than that outlined in Principle 4 of our Standards. Individuals seeking registration with the CRPO should inquire of their College if a mentorship, training or consultation relationship, rather than a formal supervisory one, as defined by our College, may satisfy the requirement. In agreeing to consult, the College would expect members to inform CRPO qualifying members that they should not indicate to clients that they are being ‘supervised’ as this could be misleading and suggest a degree of responsibility by the College member which is inaccurate. Rather it would be appropriate for them to explain that they are seeking consultation and training from a member of our College.
Post Transition Period:
The legislation only permits one to supervise individuals who are fulfilling the requirements of their own College, in our case, the College of Psychologists. Therefore, after December 31, 2019 one cannot provide supervision, as it is defined by the College, to individuals who are becoming members of another College. Please see item e) below for information about the supervision of those registered with another College, but not authorized to practice autonomously.As noted above, there is no restriction with regard to College members offering training, support, consultation and mentorship to other practitioners. While the CRPO may use the term “supervision” in their requirements for candidates, their use of the term may connote a less formal arrangement than that outlined in Principle 4 of our Standards. Individuals seeking registration with the CRPO should inquire of their College if a mentorship, training or consultation relationship, rather than a formal supervisory one as defined by our College, may satisfy the requirement.
e) Members of another regulated health profession who themselves are authorized to perform the controlled act?
Yes. If these individuals are authorized by their own College to perform the controlled act, they can do so independently or under the supervision of a member of the College of Psychologists. As with members of the College of Psychologists who are authorized to perform the Controlled Act [as per 3.c) above], in most circumstances it may be appropriate to establish a non-supervisory relationship that would afford them training, support, consultation and mentorship. If, however, there is a reason that non-supervisory supports would be insufficient, and supervision is necessary, a member of the College may enter into a supervisory relationship as outlined Principle 4 of the Standards.
4. Are there any circumstances when a member may supervise others in providing services, including performance of the Controlled Act, because a third-party payer will only cover services if they are supervised by a Psychologist or Psychological Associate?
Supervision of the controlled act of psychotherapy or any other psychological service may not be undertaken solely to facilitate third-party payment [Standards of Professional Conduct 4.1.1 (6)].
5. May I supervise a Registered Psychotherapist or Social Worker in services which fall outside of the definition of the Controlled Act?
Yes. You are permitted to supervise activities that fall outside of the definition of the Controlled Act by a Registered Psychotherapist or Social Worker or anyone else that you believe has the education, training and experience to provide those services under your supervision.
6. Can exceptions to the restrictions on performance or supervision of the Controlled Act be made for clients who require services in remote communities or who would be affected because a therapist is no longer eligible for supervision?
The legislation does not provide for any exceptions and the College cannot recommend or condone any activity that would not be permitted by legislation. In assuming responsibility for the supervision of a psychological service, the supervisor has taken on responsibility for the client’s care. Where a supervisee is no longer able to provide the supervised service, the supervisor may provide client care him or herself, or help the individual to find another competent practitioner from whom they can receive services.
The College has not set out specific, concrete age boundaries between the various client populations: children and adolescents; adolescents and adults; adults, and seniors. One usually goes by conventional definitions. That is, children to age 12 or 13; adolescents to age 19 or so; adults to 65 or 70. While age is not an issue when considering providing service to a client who falls within these conventional age groups, problems can arise at the boundary ages, i.e., 12-13; 18-20; 65-70. When determining whether it is within one’s area of competence to provide service to a “boundary age” individual, many things other than just chronological age come must be considered.
The concern that arises should a member, with demonstrated competence in working with adults, decide to provide service to an older, boundary age adolescent is that one may impart to the older adolescent some adult traits, characteristics, or difficulties based on one’s training and experience. Conversely, a member may not recognize some adolescent trait, as one is approaching the client from an « adult » perspective. Issues can also arise with the use of assessment measures and intervention techniques as one may be most familiar with both the objective and subjective norms related to working with adults.
The Registration Regulation (O. Reg. 74/15) requires that members practice the profession only within those areas of the member’s competency that are authorized by the College [s. 10 (2) 1.] There is some room at the boundary ages, however, for a member to provide service to a client who might fall, by convention, just outside of one’s authorized population group. Whether a member is practicing within one’s area of competency, as required by the Regulation, is a determination a member must make on a case by case basis, based on the characteristics of the individual client.
A member whose area of competence is Clinical Psychology with adults may occasionally see a boundary age adolescent (18-20 age range), who many might consider a young adult, dependent upon the evaluation of his/her level of development and maturity. It is important to stress however, that should such requests for service become a more regular occurrence, it would be prudent for the member to one consider expanding one’s authorized population groups.
While the above information relates to a boundary age adolescent and a member whose area of competency is with adults, the principles can be applied to a member considering providing psychological service to the other boundary age client groups.
You’ve asked about situations in which you are being required to act in contravention of the Standards. The Standard requiring best efforts to affect change in the workplace relates to situations in which others in the workplace are doing things that contravene the Standards.
When attempting to address the conduct of others in the workplace, Standard 3.1.2 does require you to make the best efforts to ensure that your work setting adheres to the Standards.
If your efforts to change the behaviour of others at work meet resistance, best efforts could include presenting additional information that supports a compelling argument for the changes, writing a formal memo to those in a position to modify policies, or escalating the issue to a higher level in the organization. You would not be expected to take steps like resigning from your position and losing your livelihood, as this would be considered undue hardship.
It is different if you, as opposed to others in the organization, are required to contravene the Standards, as a failure to comply with the Standards, yourself, would constitute Professional Misconduct. For example, if an employer were to ask you to provide services outside of your authorized areas of practice and/or competence, without the opportunity for supervision, you would not be permitted to so under any circumstances.
Fortunately, it is in the best interests of most employers to support ethical practice and most of the time it is possible to affect change. If you are unable to resolve this problem with your employer on your own, it may be necessary to seek independent legal advice to discuss your range of options.
Please don’t hesitate to contact the College’s Practice Advisory service if you’d like to discuss any specific situations like the ones described above.
The Supervision standards apply to the supervision of all psychological services and psychological research is deemed to be a psychological service. In the public interest, it is important to ensure that research is conducted ethically and that it produces reliable and valid information.
Some activities which non-members perform in the course of assisting with research may not require supervision if one would not need professional education, training, and/or experience in order to perform them. For example, tasks like administratively providing and collecting self-administered questionnaires may be performed without the supervision of the nature required by the Standards. Tasks which do require professional education, training, and/or experience, like interactive administration of tests and/or interpretation of subjects’ responses, would require supervision in the manner set out in the Standards.
If you do not wish to take on the responsibilities of a supervisor, you would need to ensure that he would be satisfied with your acting as a consultant and/or trainer, but not as a supervisor as defined within the Standards of Professional Conduct for members of the College of Psychologists of Ontario. You’d have to have an agreement with him that makes it clear that you are not clinically responsible for the casework, that it’s his responsibility to evaluate any information you are providing to him and that he would need to make his own independent decisions about whether to heed any advice you give. In the event that he requires someone to assume clinical responsibility for his services, you must make it clear to him that by consulting and/or training you would not be assuming responsibility for client care.
Your question suggests that you would be supervising another professional’s “practice”. It is important to remember that clients seen under your supervision are actually considered to be your own clients and, as such, you should consider them as clients of your practice and not the supervisee’s.
There is no specific prohibition against supervising another professional with respect to the care of some individuals, without supervising the care of all of the individuals they work with. It can, however, be challenging to ensure that all of those concerned are aware of which activities you are supervising and which ones you are not. In addition to complying with the Standards relevant to supervision, you would have to be mindful of adhering to all of the other relevant Standards, including:
6.4 Public Announcements
Public announcements of psychological services and fees must be offered in the name of an
autonomous practice member of the College.
This means that you may not permit a supervisee to advertise the services which you supervise under his or her own name, and must instead advertise the supervised services as part of your own practice.
9.1.2 Members Responsible for Supervising Supervised Practice Members and Non Members
Members supervising Supervised Practice members and non-members are responsible for the security, accessibility, maintenance and retention of records.
This means that you must ensure that you have full control over the records of those clients whose services you supervise, and take possession of those files when the supervision (and your authority) ends.
11.1 Fees and Billing Arrangements
A member must reach an agreement with an individual, group, or organization concerning the psychological services to be provided, the fees to be charged, and the billing arrangements prior to providing psychological services. Any changes in the services to be provided must be agreed to by the client before the service is delivered or fees are changed. Fees must be based on the amount of time spent and complexity of the services rendered.
This means that you must be directly involved in all agreements for services, as well as fees and billing arrangements, prior to the supervisee beginning to provide service or before arrangements are changed.
All of the information above applies, regardless of whether the supervisee is a member of another health regulated profession if you are supervising them in the provision of psychological services.
The question of the release of raw test data involves an understanding and interpretation of the Personal Health Information Protection Act (PHIPA) which speaks to responding to requests for personal health information. It should be noted that the College does not provide legal advice or legal interpretations of legislation but recommends that members seek legal advice on such matters. While not providing legal advice, the College does offer some comments which may be helpful in understanding this question and informing the discussions with legal counsel
The Personal Health Information Protection Act (PHIPA) gives a client, or legal guardian, the right of access to, or the right to consent to the disclosure of, his/her personal health information. This would include much of the information in the psychology file. There are some exceptions, however, to this right. These include information that could pose a risk of harm and confidential third party information. As well, “raw test data from standardized psychological tests” [PHIPA 51.(1)] is excluded from this right. Therefore, the legislation does not appear to provide a right to access raw data.
In considering PHIPA 51.(1), it is important to recognize the distinction between a right and a permitted disclosure. There does not appear to be any statements in PHIPA that prohibit the release of “raw test data from standardized psychological tests”. The difference to be understood is between what the client may have a right to obtain, and what they may be permitted to receive. In this regard, the legislation is permissive, rather than prescriptive.
Recognizing this permissive language in the legislation, the College position related to the release of raw test data may be found in Principle 10 – Assessment and Intervention of the Standards of Professional Conduct; specifically section 10.8. This section notes that the College recommends that when the request is reasonable and appropriate, and with proper authorization, the raw data should be released to clients and others.
It is important to note that Principle 10.8 emphasizes the member’s responsibility to distinguish between raw test data from standardized psychological tests and test materials or forms. This suggests that test protocols, test items, summary sheets, etc., most of which are materials copyrighted by the publisher, should not be reproduced based on voluntary consent. Rather, one may have to recopy the information ensuring not to include any copyrighted materials. Of course, should one receive a court order, summons to appear and bring materials to court, or some other legal vehicle compelling the release of the entire file, then this could also include the raw test data protocols. In such cases, members are encouraged to consult with legal counsel and/or the test publisher.
Autonomous practice members wishing to add an area of practice or a client group must undertake training and supervision to achieve competency comparable to other members of the College who are recognized for similar practice.
Members are required to make a written request to the Registration Committee specifying the practice area or client group they wish to add and to provide detailed information about how they have or plan to acquire the knowledge and skills in this new area.
The College’s Guidelines for Change of Area of Practice, outline the process in more detail.
The Registration Committee meets approximately every other month, dates of upcoming meetings are posted on the College’s website.
The Standards relevant to supervision are only applicable to the supervision of psychological services. If your supervisory role is strictly administrative and you only do such things as approve vacation time, arrange scheduling or perform other human resources-related activities, then you would not be subject to the requirements for supervisors of psychological services. If you do supervise activities that would fall within the scope of practice of psychology, then you are required to adhere to the Standards regarding the supervision of psychological services.
Section 3 of the Psychology Act, 1991 defines the practice of psychology as:
… the assessment of behavioral and mental conditions, the diagnosis of neuropsychological disorders and dysfunctions and psychotic, neurotic and personality disorders and dysfunctions and the prevention and treatment of behavioral and mental disorders and dysfunctions and the maintenance and enhancement of physical, intellectual, emotional, social and interpersonal functioning. 1991, c. 38, s. 3.
In Canada, the practice of psychology is regulated at the provincial/territorial level. That is, each province/territory is responsible for the regulation of psychological services delivered within its borders. Within the United States, psychology is similarly regulated.
At this time, most jurisdictions regulating psychology in Canada and the US, including the College of Psychologists of Ontario, view services to be delivered in the province/territory/state in which the client is located whether such service is provided in person or through telepsychology. That is, the service is deemed to be provided where the client is, regardless of where the psychologist or psychological associate may be located. Given this, many regulatory bodies expect the practitioner to be registered/licensed in the jurisdiction in which the service is being provided.
At this time, there is some variability in the expectations of the various Canadian jurisdictions with regard to what is required of a practitioner providing services by telepsychology into their province/territory. Some may have temporary or courtesy registers which permit a member to practise within their jurisdiction for a limited period of time without formal registration with them. For members considering providing service by telepsychology into another jurisdiction, it is recommended that they contact the regulatory body of the jurisdiction into which they may be considering practising to determine what may be required of them in terms of registration/licensing or formal notification of the regulatory body for psychology. The College of Psychologists of Ontario has adopted, as advice to members, the Model Standards for Telepsychology developed by the Association of Canadian Psychology Regulatory Organizations (ACPRO). In addition, a joint task force of the Association of State and Provincial Psychology Boards (ASPPB), the American Psychological Association (APA) and the American Psychological Association Insurance Trust (APAIT) has recently developed Guidelines for the Practice of Telepsychology. The Canadian Psychological Association has also published Draft Ethical Guidelines for Psychologists Providing Psychological Services Via Electronic Media.
Members considering providing telepsychological services will find these documents very useful as they provide guidance on a variety of issues related to this type of service. This includes ensuring one is legally entitled to practise in another province, territory, or state and one is familiar with the relevant laws and regulations applicable within that jurisdiction.
If you are supervising psychological services, the public is entitled to rely on an expectation that the services delivered will meet the standards of the profession.
There are unregulated professionals providing many services in Ontario, including behavioural intervention, counselling, and rehabilitation therapy. These professionals may be providing competent and ethical work but they are not subject to rigorous entry to practice requirements, standards of conduct to comply with, mandatory quality assurance requirements or a complaints mechanism to address concerns that may arise about the services. When a College member is supervising the provision of any psychological services, the College and its members have an obligation to the public to ensure that the services meet the same standards as they would if delivered directly by the member.
If you are supervising the psychometrist, then a supervisory agreement is necessary. In institutional settings, such as school boards, hospitals, and correctional facilities, if your employment contract and the supervisee’s employment contract both address the required terms of supervision referred to in the Standards, this would be considered to constitute a supervision agreement.
Many of the elements of a supervision agreement listed within the Standards apply broadly to any situation in which supervisors take responsibility for the work done by their supervisees. Some elements of Standard 4.1.1 (5) which may be applicable to the supervision of research and other non-clinical activities include:
a) the date upon which the agreement is effective and the expected date upon which it will expire;
b) the specific duties and obligations of the supervisee;
c) any limitations imposed upon the activities of the supervisee;
d) the specific duties and obligations of the supervisor;
e) the expected frequency and length of supervision meetings;
g) contact information and emergency contact information for both the supervisor and supervisee;
h) confirmation that the supervisee will comply with all requirements under the legislation and regulations relevant to the service and the Standards of Professional Conduct (2017); and
i) identification of a plan for appropriate support for the supervisee in the event of the supervisor’s unavailability.
In institutional settings, such as Universities and hospitals, employment contracts that address the terms of supervision referred to in these Standards may be considered to constitute a supervision agreement.
Many of the elements of supervision records listed within the Standards apply only to the care of clients. Some, however, apply more broadly to any situation in which supervisors take responsibility for the work done by their supervisees. Some elements of Standard 4.1.1 (3) which may be applicable to the supervision of research and other non-clinical activities include:
a) the date and length of time of each supervision meeting;
d) a summary of discussions regarding any relevant ethical, professional and jurisprudence issues discussed at each supervision meeting;
e) a notation of any directives provided to the supervisee at each supervision meeting; and
f) a notation of any of the supervisee’s strengths and needs for further development identified at each supervision meeting;
A supervisor would be expected to make a record of any relevant ethical, professional, and jurisprudence issues discussed, directives provided, and strengths and needs for development identified during a supervision meeting. If few or none of these things were discussed at a particular meeting, then only a very brief notation including only the date and length of the meeting would be required.
The Standard is intended to ensure that there is clear agreement between the supervisor and supervisee with respect to all of the minimum elements listed in the Standards. It may be onerous to individuals make agreements that are redundant. So long as it can be demonstrated that each individual supervisor and supervisee has agreed to all of the following elements, whether directly or through a third party, you could consider that there is an agreement which meets the Standards:
a) the date upon which the agreement is effective and the expected date upon which it will expire; b) the specific duties and obligations of the supervisee; c) any limitations imposed upon the activities of the supervisee; d) the specific duties and obligations of the supervisor; e) the expected frequency and length of supervision meetings; f) the manner in which the supervisor will be directly involved in the planning, monitoring and evaluation of the services provided to clients; g) contact information and emergency contact information for both the supervisor and supervisee; h) confirmation that the supervisee will comply with all requirements under the legislation and regulations relevant to the service and the Standards of Professional Conduct (2017); and i) identification of a plan for appropriate support for the supervisee in the event of the supervisor’s unavailability.
To the extent that any of the minimum elements of an agreement listed above are not addressed, an additional agreement covering the missing elements would be required.
Because of the diversity of supervision and consultation arrangements members are involved in, the College could not possibly provide examples or templates of agreements that would cover every situation.
We encourage you to design agreements that make sense for your own particular practice that contain at least the minimum information specified in the Standards. You are also free to add any additional elements you consider important in an agreement and may use any kind of language you wish to use.
If it would help to see how some similar agreements are structured, here is a link to a few sample supervision contracts online: http://www.cfalender.com/supervision-contracts.html. These may or not be relevant or appropriate for all kinds of relationships but may provide a sense of what others’ agreements look like.
Although the Standards require you to record information that will permit the identification of each client, there is no need to use full client names, as long as it is possible for you to associate these identifiers with the clients should you need to. The use of coded names would prevent the release of unnecessary personal health information about clients to those reviewing a file for purposes related only to the supervisee.
Examples of appropriate references to clients in a supervision file include: “Discussed Interpretation of Test Scores for A.L. and asked Supervisee to correct tabulations and reinterpret with new scores” or “Discussed Supervisee’s own reaction to N.Q.’s disclosure, Supervisee discussed own discomfort with this issue and we generated a list of other possible responses, including seeking more information or waiting for the client to reflect before problem-solving. Will discuss Supervisee’s reactions to client information again following N.Q’s next session.”
When a client makes a request for his or her record, or authorizes release of it to another person, subject to the specific exceptions in privacy legislation, you must comply with the request. All information about a client that is relevant to the services provided should, however, be contained within the client record. There should be no information relevant to client care in a supervision record that would not also be found in the client’s own file.
A supervision record should contain only information relevant to the member’s supervision of the supervisee’s performance, developmental goals, progress, and challenges. It should only include incidental reference to clients to relate the narrative to specific cases.
If for any reason, you are compelled to provide a supervision record because it contains information related to a client, it would be important to ensure that information about other clients recorded in the supervision record is not disclosed without their consent or unless you are legally compelled to release it. Similarly, you should not release personal information about the supervisee without the supervisee’s consent, unless you are legally compelled to release it.
If faced with a request which leads you to believe that supervision records are specifically being sought, you may indicate that the supervision records pertain to the supervisee’s own developmental goals, training, and growth, that all client-related information is incidental to these issues, and that all client-related information is contained in the client file. Again, unless required by a court of law, you must not release supervision records unless both the supervisee and client specifically authorize you to do so.
You may supervise anyone you believe has the competence to provide services under supervision, so long as they are not performing one of the Controlled Acts as listed and described in the Regulated Health Professions Act, 1991, which include: communication of a diagnosis; applying or ordering the application of a form of energy; and, once proclaimed in force, the Controlled Act of Psychotherapy. As counselling is not a controlled act, there is no requirement that they be registered, or seeking registration, in a College.
Consultation is defined in the Standards as:
… the provision of information, within a relationship of professionals of relatively equal status, generally based upon a limited amount of information that offers a point of view that is not binding with respect to the subsequent professional behaviour of the recipient of the information.
Supervision is defined as:
…an ongoing educational, evaluative and hierarchical relationship, where the supervisee is
required to comply with the direction of the supervisor, and the supervisor is responsible for the actions of the supervisee.
In providing exclusively training and advice to other professionals, it is more likely that you are providing consultation than supervision. If this is the extent of your involvement with these individuals, adherence to the requirements under section 4.1.5., which involves clarification of the limits of your involvement as a consultant, would be sufficient and appropriate.
Your question indicates that you ‘have some input into the administration of tests and counselling’. If your input involves only making recommendations to other practitioners who take responsibility for the decision about whether to accept the recommendations, this would be consistent with the role of a consultant. If, however, “input” means directing which tests and counselling interventions will be used, and the recipients of the input are required to follow your directions, it may be that you are providing supervision and would be bound to adhere to the Standards regarding supervision of non-regulated professionals. If you are interpreting test results yourself, then you are considered to be actually providing a psychological service to the clients, and you are expected to adhere to all of the Standards which apply to the direct provision of psychological services.
Providing training does not necessarily make a relationship supervisory. A relationship in which you have been specifically asked to provide training, or a consulting relationship which may have a training component, only becomes a supervisory relationship if it becomes evaluative and hierarchical and when the person receiving information from you is required to do as you instruct. In the kind of consultation situation, you have described it is particularly important to ensure that an agreement makes it clear that you are not taking on responsibility for client care and that that responsibility is exclusively the consultee’s.
Making case specific recommendations to behavior therapists, advising with respect to the development of processes, and discussing general issues, are activities which are consistent with the role of a consultant, so long as it is understood that the recipients of the recommendations and advice are fully responsible for deciding whether to implement your recommendations.
If you are in a relationship with the behavior therapists that is educational, evaluative, and hierarchical, and they are required to comply with your direction, you would be considered to be supervising them.
Consultants are typically in the role of an external contributor to case discussions, where the recipients of the consultant’s ideas are free to either accept or reject them. If you are in the role of a consultant, while you may be providing advice to those making decisions about client care, you should not actually participate in making the decisions (e.g., “have a vote”), even when the responsibility for decision-making is shared.
Consultation is defined as:
… the provision of information, within a relationship of professionals of relatively equal status, generally based upon a limited amount of information that offers a point of view that is not binding with respect to the subsequent professional behaviour of the recipient of the information.
If this description fits your role with respect to the treatment team then it is likely that you would be considered a consultant and are required have a clear and formal agreement delineating responsibility for client care which spells out that the person receiving your consultation retains full responsibility for client care, in accordance with Standard 4.1.5.
If you are a participant in the actual clinical decision making with respect to the clients, as opposed to being simply a resource for the decision-makers, then you are more than a consultant and have the same obligations as any member of the College providing services to a client, in a way that is analogous to an assessor or file reviewer who does not provide intervention but must comply with all of the Standards with respect to client care.
There is no reason you cannot have an agreement that multiple parties can sign onto, so long as it includes everyone with whom you require an agreement. You could update this agreement whenever someone joins or leaves the team.
It would be reasonable to understand “formal” in this context to mean that contacts with the consultee(s) have been arranged, or are expected to occur in the future, specifically for the purpose of consultation, where consultation is defined as:
… the provision of information, within a relationship of professionals of relatively equal status, generally based upon a limited amount of information that offers a point of view that is not binding with respect to the subsequent professional behaviour of the recipient of the information.
This would be different than the regular discussions which frequently occur between professional peers on either an ad hoc basis or at team meetings or case conferences. It would be reasonable to consider a consultation arrangement to be “ongoing” if the participants expect to have future contact for the purpose of consultation.
If all members of the discussion are simply exchanging ideas, and you were not designated to make specific recommendations to others by virtue of your specialized expertise, it would not be considered “consultation”, which is defined as:
… the provision of information, within a relationship of professionals of relatively equal status, generally based upon a limited amount of information that offers a point of view that is not binding with respect to the subsequent professional behaviour of the recipient of the information.
Rather, it could be simply understood as team discussion or team development.
If, however, a relationship is established with specific individuals or groups, where you are identified as a person who is designated to provide advice or information regarding psychological matters, and there were plans for you to meet with them to provide advice or information more than once, then it would be considered to be formal, ongoing consultation.
There have been no changes to the Standards with respect to members limiting their services to their authorized client populations. We have tried, in revising the Standards, to make more members aware of the advice we provide about both the limits to authorized client populations and authorized areas of practice.
Members are still required to limit their services to their authorized populations and areas of practice. The College has never set age cutoffs, with the belief that members will use good judgment to determine whether a person is a child, adolescent, adult, or senior. Those distinctions should be based upon whether, in the member’s judgment, the client’s abilities, life situation, and challenges are consistent with those commonly associated with a particular group. We’ve provided some examples in the Practical Applications to Standard 5.1 contained within the Standards.
If you are not authorized to work with seniors, it would not be appropriate to take on a client facing age-related mental health challenges such as cognitive decline or social isolation.
If deciding whether to continue ongoing treatment with a client who has recently begun to experience the adverse effects of old age, it would be a good idea to refer him or her to someone authorized to work with seniors and, until this has occurred, seek consultation from someone with the specific training, skills and experience and who is authorized to work with seniors.
If an existing client is at a chronological age when age-related difficulties could reasonably be expected but are not yet occurring, it may be reasonable to still consider the client an “adult”. For example, if the client continues to work productively, live independently, has a vigorous fitness routine, is free from age-related health concerns, has meaningful and satisfying close relationships, etc., he or she need not be categorized as a “senior” for the purposes of the Standards, even if his or her age exceeds a commonly applied age marker such as 65.
The clients receiving services directly from your supervisee are considered to be your clients. As such, the client file is actually yours even while in the possession of a supervisee under your direction; this is the case with respect to files of clients seen by members of the College with Certificates of Registration Authorizing Supervised Practice as well as non-members of the College. You may decide that, rather than keeping client files in your possession while services are being provided, your supervision would extend to ensuring that the supervisee maintains the files in a secure, confidential and accessible manner, in accordance with the Standards and the applicable legislation. When the supervision period ends, the record of services which you had always been responsible for remain your responsibility. Given that you will not have authority over the conduct of the former supervisee, you must personally ensure that the records remain secure, confidential and accessible in the manner required by the Standards.
The Standards do not specifically prescribe what you must do with supervision files when you leave an organization in which you are providing supervision. In most cases, supervision of services to the clients of the organization would be considered an activity of the organization which is performed by the supervisor. If this is the case, the file likely belongs to the organization and it would make sense for the file to be left in the organization’s care and dealt with in accordance with the privacy legislation applicable to the organization. It is important to make the best efforts in these situations to ensure that the organization will retain the files for at least two years, as this is the prescribed retention period for supervision files when they belong to individual members who are not carrying out supervision in an organizational context. To use the analogy of a human resources file, if you would leave a human resources record with the organization in which you managed staff, then it’s likely that you would be expected to leave the record of supervision with the organization within which the supervision was provided. With respect to any information about an identifiable client in the files, the organization would, in most cases, be considered the Health Information Custodian and would be responsible for ensuring that the requirements of the Personal Health Information Protection Act are met.
The prohibition against fee splitting has been removed from the Standards but the prohibition against paying for referrals remains in force. The Professional Misconduct Regulation still strictly prohibits:
- Receiving or conferring a rebate, fee or other benefit by reason of the referral of a client from or to another person (Section 1.26)
Many people found the language used to address the practice of fee splitting in the previous version of the Standards difficult to understand. The College decided that concerns underlying the former specific fee splitting rule are already adequately addressed within the Professional Misconduct Regulation, which prohibits:
- Providing a service that the member knows or ought to know is not likely to benefit the
Client (Section 1.9); and - Practising the profession while the member is in a conflict of interest (Section 1.10);
and by the following requirements which have been carried forward from the previous Standards to the new ones:
- Fees must be based on the amount of time spent and complexity of the services rendered (section 11.1); and
- A member must not exploit persons over whom he/she has supervisory, evaluative, or other authority such as clients, students, supervisees, research participants, or employees (section 13.4(2)).
As a supervisor, you are providing a psychological service and it is important that your own fee structure for this service complies with the requirement that your fees are based on the amount of time you spend providing the service and the complexity of the service you are providing. Charging a percentage of fees collected or the number of sessions a supervisee has with a client may not correspond to the amount of time you are providing supervision. Charging a flat fee for a time period, without regard to the specific number of hours spent within that time period, would also be inconsistent with the standard and would have the potential to also violate the prohibition against exploitation of supervisees (section 13.4(2), as a supervisee could possibly be charged for supervision which was out of proportion to the time spent.
The prohibition of fee splitting was difficult to understand and misunderstood by many, so it was decided that, because concerns about the adverse consequences of fee splitting are addressed elsewhere in the Standards and the Professional Misconduct Regulation, that the Standard regarding fee splitting would be omitted from 2017 version.
The Professional Misconduct Regulation still strictly prohibits:
-
Receiving or conferring a rebate, fee or other benefit by reason of the referral of a client from or to another person (Section 1.26)
-
Providing a service that the member knows or ought to know is not likely to benefit the client (Section 1.9); and
-
Practising the profession while the member is in a conflict of interest (Section 1.10)
Additionally, the Standards still require that:
-
Fees must be based on the amount of time spent and complexity of the services rendered (section 11.1); and
-
A member must not exploit persons over whom he/she has supervisory, evaluative, or other authority such as clients, students, supervisees, research participants, or employees (section 13.4(2)).
As long as the practice you are describing does not occur in a supervisory relationship and your practice is compliant with respect to all of the above, you are now able to enter into percentage based arrangements.
The College has adopted the Association of Canadian Psychology Regulatory Organizations (ACPRO) Model Standards for Telepsychology Service Delivery. The Model Standards define Telepsychology as “the use of information and communications technology to deliver psychological services and information over large and small distances”. Practice within psychology using this modality would include all client-centered services, consultation, supervision of students/professionals/colleagues, and the education of the public and/or other professionals delivered to individuals outside of Ontario.
A telephone (landline or mobile) would be considered “communications technology”. While some of the items within the “Use of Technology…” section of the Standards may not be relevant to simpler, older technologies, some items would be relevant and applicable to even ‘lower-tech’ devices, including a corded or land-line telephone. Examples of requirements applicable to the use of all technologies in service provision would include the need to obtain authorization from the relevant jurisdiction before providing services to someone who is located outside of Ontario, ensuring the privacy of the person you are communicating with, and having contingency plans in the event of a technological failure.
Pour les employeurs, les assureurs et les tiers payeurs
Renseignements pour les tiers payeurs
Il existe une certaine confusion sur la question de savoir qui peut fournir des services de psychologie en Ontario et qui peut facturer de tels services. Les lettres que voici ont pour but d’apporter une réponse claire à ces questions.
Pour exercer la psychologie en Ontario, il faut être titulaire d’un certificat d’inscription de l’Ordre des psychologues de l’Ontario, qui réglemente la profession de psychologue. En vertu de la Loi de 1991 sur les professions de la santé réglementées et de la Loi de 1991 sur les psychologues, l’Ordre inscrit deux catégories de professionnels autonomes : les psychologues et les associés en psychologie.
Les psychologues et les associés en psychologie qui sont titulaires d’un certificat d’inscription autorisant l’exercice autonome de la psychologie peuvent fournir des services sans supervision dans leur champ de compétence, et peuvent facturer ces services. Bien que le certificat d’inscription de la plupart des membres de l’Ordre ne soit pas assorti de conditions ou de restrictions, certains d’entre eux ont un certificat assorti de conditions et de restrictions et ceux-ci doivent exercer la profession conformément aux conditions et restrictions qui leur sont imposées.
Pour obtenir un certificat d’inscription afin de pouvoir exercer la psychologie, il faut satisfaire aux conditions suivantes :
- répondre à des exigences rigoureuses en matière d’éducation et de formation ;
- posséder une expérience professionnelle supervisée acceptable ;
- réussir un examen normalisé écrit qui évalue l’ensemble des connaissances en psychologie et qui est administré partout au Canada et aux États-Unis ;
- réussir un examen écrit qui évalue les capacités du candidat à mettre en application ses connaissances de la jurisprudence, de la déontologie et des normes professionnelles pour exercer en Ontario ; et
- réussir un examen oral conçu pour évaluer si le candidat est prêt à exercer la profession de façon autonome.
Après avoir obtenu leur certificat d’inscription, les membres de l’Ordre doivent exercer la profession conformément aux lois et aux règlements applicables et conformément aux normes de conduite professionnelle, aux lignes directrices professionnelles et au code de déontologie établis.
Seuls les membres de l’Ordre des psychologues de l’Ontario sont autorisés à offrir des services de psychologie en Ontario ou à employer le titre de « psychologue » ou d’« associé en psychologie ». De plus, seuls les membres de l’Ordre sont autorisés à utiliser les termes & #171; psychologie » ou & #171; psychologique » ou toute abréviation ou variation de ces termes et titres lorsqu’ils décrivent leurs services. Les psychologues et les associés en psychologie peuvent également s’identifier en ajoutant la désignation C.Psych. ou C.Psych.Assoc. après leur nom.
L’Ordre tient un tableau de tous ses membres actuels. Pour obtenir des renseignements sur un psychologue ou un associé en psychologie, vous pouvez consulter le tableau public ou vous adresser à l’Ordre par téléphone au (416) 961-8817 ou par courriel à cpo@cpo.on.ca
L’Ordre a reçu des demandes de renseignements portant sur le statut des associés en psychologie qui fournissent des services conformément à des lois telles que l’Annexe sur les indemnités d’accident légales (AIAL) et à d’autres programmes d’assurances publics et privés. En 1996, dans une lettre envoyée à M. Sampson, député provincial et adjoint parlementaire au ministre des Institutions financières, le registrateur de l’Ordre a demandé de préciser qui sont les fournisseurs de services aux termes de l’AIAL. Voici ce que M. Sampson a répondu :
« J’ai demandé au personnel juridique de revoir la définition contenue dans l’Annexe sur les indemnités d’accident légales (AIAL) et de déterminer si la définition de psychologue englobe les associés en psychologie.
J’ai le plaisir d’affirmer que la définition du terme psychologue figurant dans l’AIAL inclut les associés en psychologie. Aux termes de l’AIAL, un ‘psychologue’ est une personne autorisée par la loi à exercer la psychologie. Comme la Loi de 1991 sur les psychologues autorise les psychologues et les associés en psychologie à exercer la psychologie, la définition donnée par l’AIAL s’applique aux psychologues et aux associés en psychologie. & #187;
L’Ordre a récemment demandé au ministre fédéral des Finances de préciser si les associés en psychologie sont autorisés à attester l’admissibilité au crédit d’impôt pour les personnes handicapées. Dans sa lettre du 31 janvier 2007, voici ce que dit M. James Flaherty :
« Je crois comprendre que la Loi de 1991 sur les psychologues de l’Ontario autorise les psychologues et les associés en psychologie à exercer la psychologie. Par conséquent, les titulaires de ces deux titres sont autorisés à attester les déficiences des fonctions mentales nécessaires aux activités de la vie courante pour les besoins de l’admissibilité au crédit d’impôt pour les personnes handicapées.
Mes représentants ont communiqué avec leurs collègues de l’Agence du revenu du Canada pour leur communiquer cette précision. Les changements voulus ont été apportés aux pratiques administratives de l’Agence du revenu du Canada afin que les associés en psychologie soient autorisés à attester les déficiences des fonctions mentales nécessaires aux activités de la vie courante. & #187;
Bref, les psychologues et les associés en psychologie sont des membres de l’Ordre des psychologues. Qu’ils soient titulaires de l’un ou l’autre de ces titres, les membres de l’Ordre sont des professionnels qualifiés pour exercer la psychologie en Ontario.
Si vous avez des questions au sujet des psychologues ou des associés en psychologie, ou sur tout autre aspect de la réglementation et de l’exercice de la psychologie en Ontario, veuillez vous adresser à l’Ordre.
Financement de la thérapie pour les victims d'abus sexuels
Under the legislation, a person may be eligible for funding if it is alleged, in a complaint or report, that they were sexually abused by a member while a client of the member.
The legislation sets the maximum amount of funding that can be awarded as the amount that the Ontario Health Insurance Plan (OHIP) would pay for 200 half-hour sessions of individual out-patient psychotherapy with a psychiatrist on the day the person becomes eligible. Currently, a total amount of $17,370 in funding is available. If OHIP or a private insurance plan covers some of the costs, the College would only pay the amount not covered.
Yes. The legislation specifically states the funding must be used only to pay for therapy or counselling and must be paid to the therapist or counsellor directly. The College will not pay for missed appointments. As well, funds from the program cannot be used to pay for travel, accommodation or other incidental costs even if they are incurred directly as a result of therapy.
Funding is available for up to five years from the time an application is approved by the Client Relations Committee or, if therapy to address the effects of sexual abuse began before such approval was granted, five years from day upon which the funded therapy began.
No. Any therapist or counsellor may be selected, if:
(a) it is confirmed that they have not at any time or in any jurisdiction been found guilty of professional misconduct of a sexual nature or been civilly or criminally liable for an act of a similar nature; and
(b) the therapist or counsellor is not a member of the client’s family.
No. The Committee reviews documents only.
The Client Relations Committee requires sufficient information to be satisfied that the criteria for eligibility have been met. The College recognizes however, that the information provided is very personal and sensitive. To this end, the Client Relations Committee will access only the minimum amount of information required to adequately undertake its review. An applicant’s surname will not be shared with the Committee and will be known only by College staff presenting the application to the Committee and processing the payments.
Applicants will be asked to keep confidential all information obtained through the application for funding process, including the fact that funding has been granted and the reasons, if any, given by the Committee for granting the funding. Furthermore, a decision by the Committee concerning eligibility for funding does not constitute a finding against the member and shall not be considered by any other Committee of the College dealing with the matter. Other College processes, including investigation and hearings may remain ongoing even during the funding application process and while funding is being provided.
Individuals who wish to apply for funding for therapy or counselling under this program, may contact the Deputy Registrar, Mr. Barry Gang. His contact information is available below. Mr. Gang will answer any further questions applicants may have and will provide assistance in applying for funding.
Applicants will be asked to provide a written statement from the therapist or counsellor to the Client Relations Committee indicating:
(a) confirmation that the therapy or counselling is being provided to the client and that the funds are being devoted only to the therapy or counselling;
(b) a short description of the therapy or counselling to be offered;
(c) the fees to be charged for the service;
(d) whether the therapist or counsellor has liability insurance; and
(e) the details of the therapist’s or counsellor’s training and experience and whether the therapist or counsellor is a member of a Regulated Health Profession;
If the therapist or counsellor is not a Regulated Health Professional, the applicant will be asked to sign a document indicating that they understand that the therapist or counsellor is not subject to professional discipline.